Key Takeaways
- Tirzepatide can cause nausea by slowing gastric emptying, making large or heavy meals more likely to trigger symptoms.
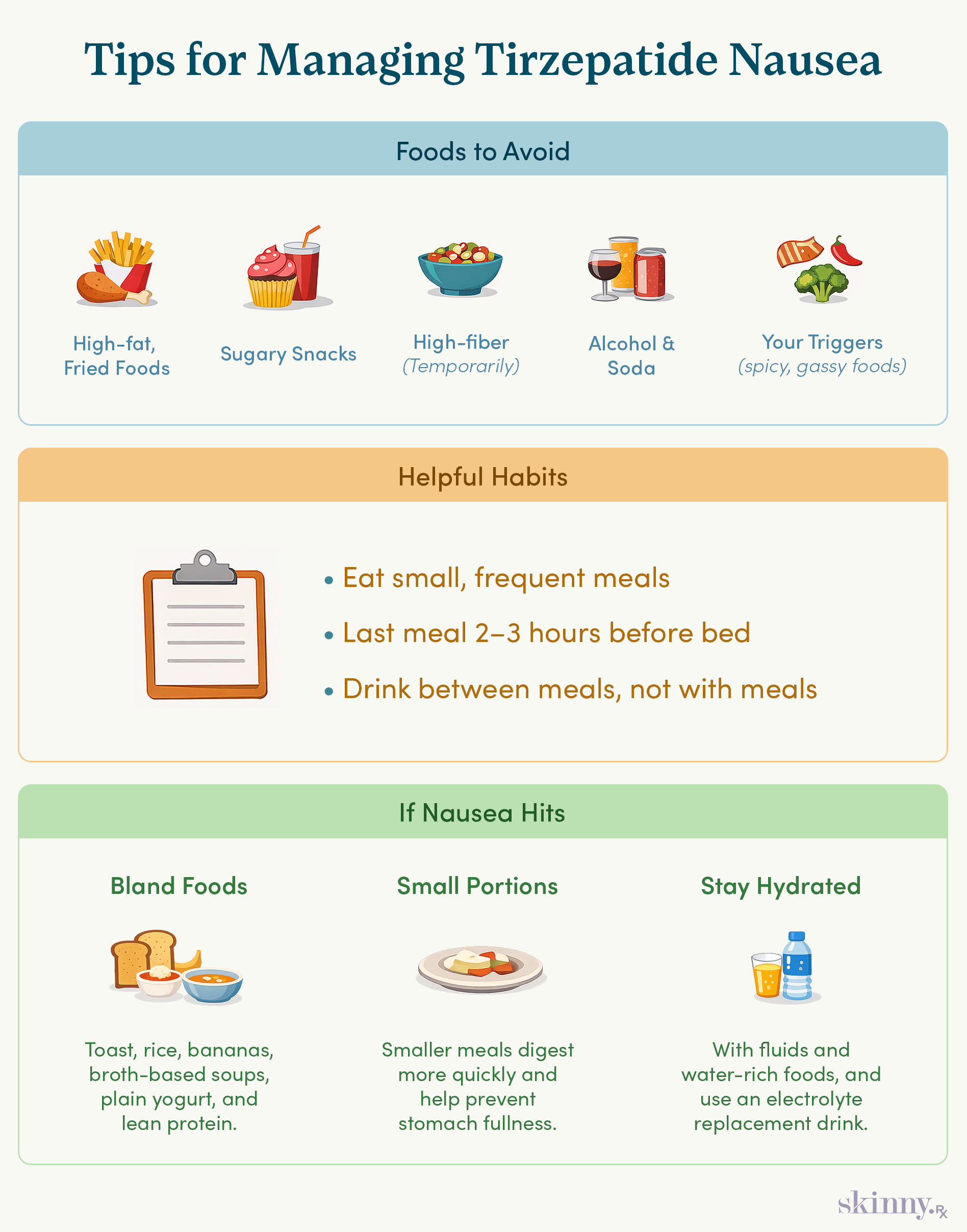
- High-fat, sugary, high-fiber, carbonated foods and alcohol are common triggers and are best limited, especially during dose increases.
- Smaller, more frequent meals, avoiding food close to bedtime, and separating drinks from meals can help reduce nausea.
- When nausea is severe, bland, low-fiber foods and liquid nutrition can help maintain intake without worsening symptoms.
- Tirzepatide-related nausea is usually temporary and manageable, but hydration and medical guidance are important if symptoms persist or include vomiting.
If you are just starting on tirzepatide or recently increased your dose, you may be experiencing nausea, which is one of the most common side effects of this medication.
Approximately one in three people taking tirzepatide will have nausea. Other common side effects include diarrhea, constipation, and vomiting.
The good news is that nausea tends to be manageable and resolves within a few weeks for most people. Plus, certain tweaks to your diet, both what you eat and when, can help to curb this unpleasant side effect.
Why Certain Foods Trigger Nausea on Tirzepatide
The Role of Delayed Gastric Emptying
Tirzepatide works by mimicking two hormones, GIP and GLP-1, which signal the brain that you are full and slow the rate of gastric emptying, or how quickly a meal leaves the stomach and enters the small intestine.
This helps you feel fuller longer after eating, which is one of the ways tirzepatide helps with weight loss. The downside is that delayed gastric emptying can trigger nausea, as well as other side effects like heartburn.
Why Your "Old" Diet No Longer Works
Since tirzepatide changes your digestion in fairly significant ways, your old eating patterns may no longer serve you well. For example, if you are someone who usually eats one or two large meals in the day, and those meals tend to be higher in fat, it may be time to adopt a new eating pattern centered on small, frequent, nutrient-dense meals.
Hidden Triggers: It’s Not Just What You Eat, But How
The Danger of Large Portions
Large, high-fat meals can easily trigger nausea as they take a longer time to leave the stomach and enter the small intestine, regardless of whether you are taking tirzepatide. Start by consuming smaller meals more frequently throughout the day, such as every 2-3 hours.
For example, try having a small meal or snack at 8:00 AM, 11:00 AM, 2:00 PM, 5:00 PM, and 7:00 PM. Smaller meals are digested more quickly than larger ones, so your stomach does not become uncomfortably full.
Eating Too Close to Bedtime
Next, aim to have your last meal of the day a few hours before bedtime. Lying down soon after eating can trigger various gastrointestinal symptoms, including nausea and heartburn.
For example, if you typically go to bed around 9:00 PM, have your last meal or snack by 7:00 PM. This will allow your body sufficient time to digest the meal so that it has passed from the stomach to the small intestine by the time you lie down. If you become physically hungry closer to bedtime, choose a small, easily digested meal such as a small Greek yogurt or 4 ounces of milk.
Additionally, a short walk after a meal can help to stimulate peristalsis (the contractions of the muscles of your gastrointestinal tract). This can aid the digestive process and prevent your stomach from feeling overly full at bedtime.
Avoid Beverages at Mealtimes
Avoiding beverages at mealtimes can also help to prevent the stomach from becoming overly full. Aim to consume plenty of fluids throughout the day; this is especially important if you are also experiencing any vomiting. But aim to stagger your fluid intake between your meals.
For example, if you’re having your first meal of the day at 8:00 AM, have any beverages (e.g., water, your morning cup of coffee or tea) at 7:00 AM. If your second meal of the day is at 11:00 AM, have your beverages between 9:00 AM and 10:00 AM.

Doctor-Guided Medical Weight Loss
Learn how prescription GLP-1 medications like semaglutide or tirzepatide may support weight loss when guided by a licensed medical provider and tailored to your health history.
The Top Foods to Avoid to Prevent Nausea
Limiting or avoiding certain foods can also help to combat nausea. The good news is that tirzepatide may not only decrease food cravings overall, but may specifically decrease cravings for foods high in fat and sugar — two common nausea triggers.
High-Fat and Fried Foods (The Slowest to Digest)
High-fat meals take a longer time to digest compared to low-fat meals. This is due to the fairly complex chemical structure of triglycerides, the main form of fat in foods, as well as the release of the hormone cholecystokinin (CCK), which delays the rate of gastric emptying, similar to GIP and GLP-1.
Limit or avoid high-fat foods, such as fried foods, fatty cuts of meat, sour cream, ice cream, and hard cheeses. Fats used in cooking, such as oils or butter, should also be used in moderation.
Lastly, even though they contain healthy unsaturated fats, nuts, seeds, nut butters, and avocados should be limited; once your nausea resolves, these are excellent nutrient-dense foods to incorporate in your diet.
Sugary Treats and Refined Carbs (The Osmotic Effect)
Next, foods high in sugar or refined carbohydrates can also trigger nausea. When a high sugar meal enters the stomach, it has an osmotic effect of pulling water into the gastrointestinal tract from the body.
This slows gastric emptying, which may trigger nausea alone. Plus, meals high in sugar and refined carbohydrates may cause blood sugar levels to spike and drop, which can also trigger nausea.
Limit or avoid foods high in added sugars, such as sugar-sweetened beverages (e.g., sodas, sweetened teas and coffee drinks, lemonade, energy drinks), candy, ice cream, and baked goods.
Fiber (Temporarily)
Although fiber is highly beneficial to your overall health, it may also worsen nausea by slowing the rate of gastric emptying.
Limit your intake of high-fiber foods until your nausea subsides, which includes beans, legumes, nuts, and seeds. Then, you can incorporate these nutritious foods back into your diet.
Note that constipation can further delay gastric emptying and worsen nausea. Talk to your physician if you are experiencing both constipation and nausea about how they can best be managed.
Once your nausea has subsided, fiber is a key nutrient for preventing or treating long-term constipation.
Carbonated Beverages and Alcohol
For some people, carbonated beverages may trigger nausea due to resulting gas, bloating, heartburn, or a sensation of fullness. Alcohol may also worsen nausea by irritating the lining of the gastrointestinal tract, inducing spikes and drops in blood sugar levels, or causing dehydration.
Choose water, unsweetened teas, and low-fat or fat-free milk as your primary beverages. Lactose-free dairy products may be easier to digest for some people. While all beverages, including alcohol, juice, and coffee, can be included in moderation, limiting these may be helpful until your nausea subsides.
Trigger Foods
Foods that trigger nausea tend to be fairly individualized, so take note of the foods that have you feeling particularly ill. Common triggers include spicy foods, sulfur-containing cruciferous vegetables (e.g., cabbage, broccoli), or those with a strong odor.
Keep in mind that nausea tends to resolve within a few weeks for most people on tirzepatide, so you can reincorporate these foods in your diet once the nausea has resolved.
The "Emergency" Nausea Diet: What to Eat When You Feel Sick
If your nausea is especially severe, prioritize bland, low-fiber, water-rich, easily digested foods to keep yourself nourished. Palatable or appetizing foods may include:
- Clear, broth-based soups, e.g., chicken noodle soup
- Low-fiber fruits and vegetables, e.g., bananas, melons, potatoes
- Lean protein, e.g., chicken, turkey, fish
- Grains, e.g., toast, low-fiber cereal, white rice
- Plain yogurt, low-fat or fat-free
Liquid Nutrition: When Solids are Too Much
When you can’t tolerate a solid meal, a liquid meal is a perfectly reasonable substitute. Focus on small portions (e.g., 8 fl oz), as large volumes of liquid in the stomach can trigger nausea. Examples may include:
- Smoothies made with low-fiber fruits, vegetables, and plain yogurt
- Clear, broth-based soups
- Popsicles made with low-fiber fruits and plain yogurt
Precautions for Vomiting
Though vomiting is far less common with tirzepatide than nausea, it is a potential side effect with this medication. Untreated vomiting can cause dehydration and electrolyte imbalances.
If you are experiencing vomiting, hydrate with fluids and water-rich foods, use an electrolyte replacement drink, and contact your doctor if your symptoms are particularly severe or last longer than 24 hours.
Practical Tips for Dosage Day Success
In summary, these practical tips can help to prevent or treat nausea with tirzepatide:
When to Eat
- Consume small, frequent meals every 2-3 hours throughout the day.
- Avoid lying down after eating.
- Drink beverages separately from your meals.
What to Eat
- Choose foods low in fat, added sugars, and fiber.
- Avoid trigger foods, which may vary from person to person.
Helpful Reminders
- Tirzepatide-induced nausea is typically short-term and manageable for most people. Though you may need to make significant changes to your diet, you can reset once your nausea has subsided.
- If your nausea is accompanied by vomiting, take care to hydrate well, supplement with electrolytes, and contact your physician if your symptoms are particularly severe or last longer than 24 hours.
Weight loss and side effects like nausea can feel overwhelming, and having the right guidance can make a meaningful difference. At SkinnyRx, you can take a brief assessment to learn about doctor-prescribed and guided medication options like tirzepatide and semaglutide. You’ll also gain access to ongoing support, resources, and a community designed to help you navigate your weight loss journey.


 Medically Reviewed
Medically Reviewed



