Key Takeaways
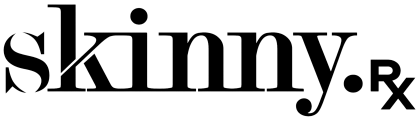
- Prediabetes is a common, often symptomless condition driven by insulin resistance that can progress to type 2 diabetes without timely intervention.
- Insulin resistance develops when cells stop responding properly to insulin, causing elevated blood sugar and increased strain on pancreatic beta cells.
- Semaglutide may help slow or reverse prediabetes by promoting weight loss, supporting insulin secretion, and stabilizing blood sugar alongside lifestyle changes.
- Clinical trials show that many people with prediabetes who use semaglutide return to normal blood sugar levels, especially when combined with diet and exercise.
- Long-term prediabetes prevention depends on sustainable habits such as regular physical activity, balanced nutrition, and ongoing care with a healthcare provider.
Most of us have probably heard about type 2 diabetes, a condition where the body can’t maintain healthy blood sugar levels. But this condition’s precursor, prediabetes, isn’t talked about as often, even though it’s incredibly common.
Prediabetes affects at least one in three adults, and the condition may be reversible with the right treatment plan. That plan may include semaglutide for prediabetes prevention.
Semaglutide is a medication that mimics GLP-1, a naturally occurring hormone that regulates appetite and blood sugar levels. Thanks to its effect on blood sugar, two name-brand semaglutide options, Ozempic and Rybelsus, are FDA-approved for type 2 diabetes.
In clinical trials, semaglutide has also been associated with a prediabetes reversal and a higher likelihood of returning to normal blood sugar levels. Continue reading to learn more about how semaglutide, when combined with lifestyle changes, may stop the progression of prediabetes to type 2 diabetes.
Understanding Prediabetes: The Critical Window for Prevention
If someone has prediabetes, their blood sugar levels are higher than what’s considered healthy but not high enough to be classified as type 2 diabetes. It’s a common, serious condition that is sometimes reversible. In fact, prediabetes is often thought of as a critical window for diabetes prevention.
What Prediabetes Means for Your Health
If it’s not reversed, prediabetes might turn into type 2 diabetes within five years. Type 2 diabetes is a serious condition where the body can’t use insulin as intended, which can be life-threatening if left untreated. When someone treats diabetes, they may still experience symptoms such as fatigue, blurred vision, numbness in their hands, increased thirst, and increased hunger.
Prediabetes also increases the risk for other health conditions:
- High blood pressure
- Heart disease
- Kidney failure
- Metabolic syndrome
- Nonalcoholic fatty liver disease
- Obesity or excessive weight gain
- Unhealthy cholesterol levels
While prediabetes is common and may lead to serious health risks, it’s difficult to diagnose since it’s often symptomless. As a result, doctors diagnose prediabetes based a blood test on that assesses blood sugar levels. Risk levels, such as being overweight or obese or living a sedentary lifestyle, are what doctors used to identify who should be screened for prediabetes.
The Centers for Disease Control and Prevention even has a prediabetes test that determines a risk estimate. A high risk level on that test indicates someone may benefit from undergoing laboratory testing for prediabetes.

Expert-Guided, Sustainable Weight Loss
Discover how proven medications such as semaglutide or tirzepatide, combined with expert support, can help you reach lasting weight loss results.
The Silent Threat: How Insulin Resistance Paves the Way for Diabetes
When we eat, our bodies break down food into sugar that enters the blood stream. That “blood sugar” can not be absorbed as is by our bodies’ cells. To help, the pancreas, an internal organ located in the abdomen, creates insulin. Insulin is a naturally occurring hormone that helps the body’s cells absorb blood sugar and use it for energy. The pancreas also contains beta cells, which regulate how much insulin is produced.
If blood sugar levels remain high for many years, the body’s cells become less responsive to insulin, which is known as insulin resistance. In response, those beta cells increase insulin production. Yet over time, they can’t keep up, and blood sugar rises, which is what then triggers type 2 diabetes.

Early screening for diabetes is important because you can’t improve what you don’t measure. Lifestyle changes are first-line for prediabetes, but for patients at higher risk or struggling to make progress, GLP-1 medications can be a valuable tool.
–
Dr. Daniel McGee, Board-certified Family Medicine Physician
The Science of Prevention: How Semaglutide Intervenes
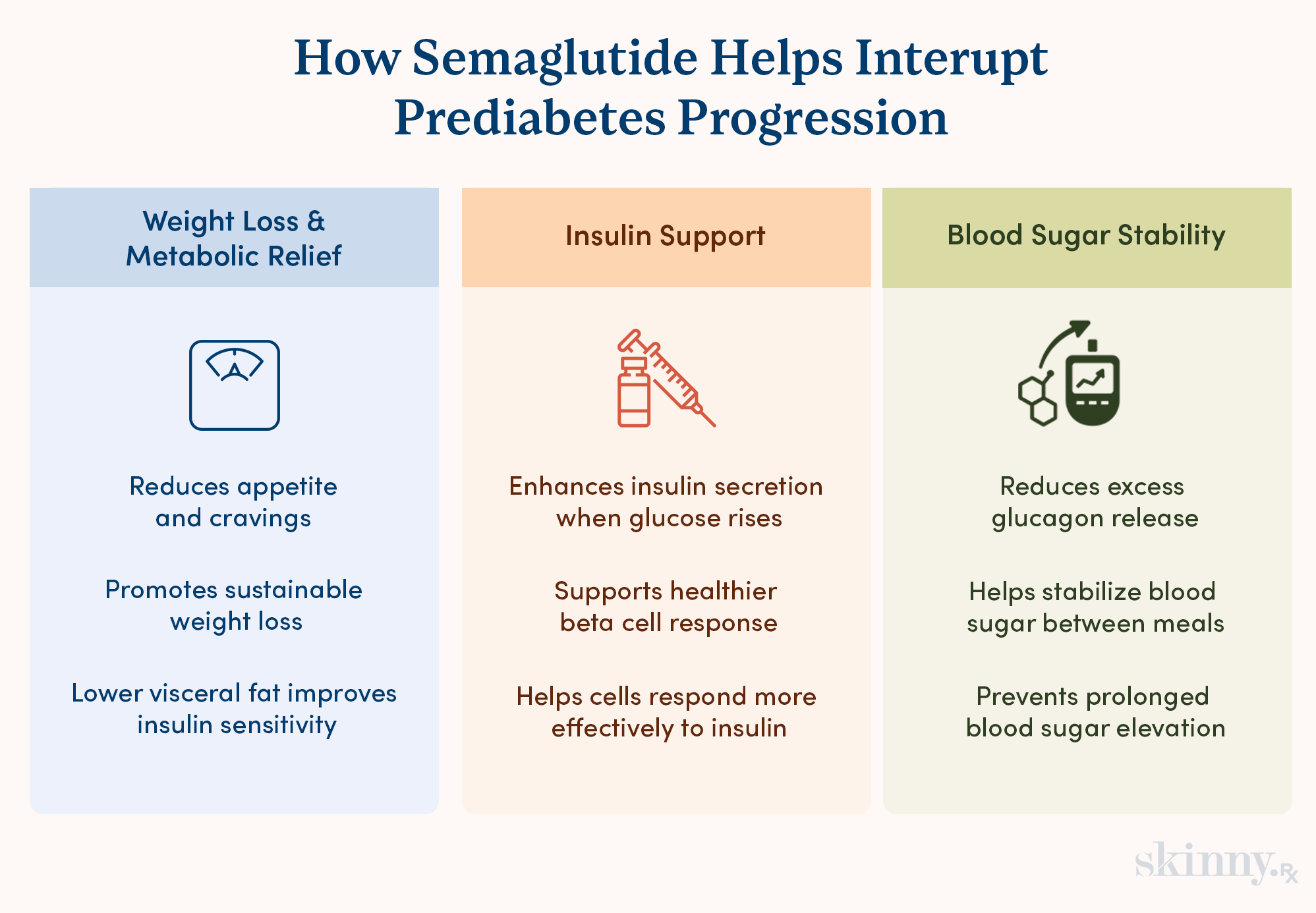
Semaglutide facilitates multiple health benefits at once. For prediabetes specifically, three of semaglutide’s benefits may help stop the progression: weight loss, enhanced insulin secretion, and stable blood sugar levels.
Weight Loss: Reducing Visceral Fat and Improving Metabolic Health
Being overweight or obese is a risk factor for prediabetes and type 2 diabetes. Since semaglutide mimics the hormone GLP-1, which regulates appetite, it helps someone feel full for longer, reduces cravings for ultra-processed foods, and slows gastric emptying. In turn, these effects often result in weight loss. In some studies, people who take semaglutide experience up to 15% weight loss in 68 weeks.
Enhancing Insulin Secretion
GLP-1s also plays a role in insulin production. Researchers are unsure why this is, but a leading theory suggests GLP-1s help regulate beta cell activity. This would mean that semaglutide may help provide sufficient amounts of GLP-1 for beta cells to produce appropriate insulin levels.
Stabilizing Blood Sugar: Counteracting Glucagon’s Effects
To make sure blood sugar remains steady throughout the day, the body produces glucagon between meals. Alpha cells in the pancreas secrete glucagon between meals. That glucagon then signals to the liver that it’s time to release stored glucose, which raises blood sugar levels.
You can think of insulin and glucagon as two kids on a see-saw; they work opposite of each other so that blood sugar decreases during and right after meals (thanks to insulin), and levels increase between meals, giving the body steady energy levels (due to glucagon). Normally, insulin suppresses glucagon after meals.
Yet in those with prediabetes, that signaling is impaired and glucagon stays inappropriately high, meaning the see-saw isn’t working as intended. Semaglutide decreases glucagon secretion, aka the release of glucagon, providing a chance to level out blood sugar levels. Stable blood sugar levels, in turn, help reverse prediabetes.
Clinical Evidence: Semaglutide's Impact on Diabetes Incidence
There’s a growing body of evidence to support semaglutide’s role in reversing prediabetes:
- In the STEP 1 trial, 84.1% of those with prediabetes who took semaglutide reverted for normoglycemia (normal blood sugar levels) within 68 weeks, compared to 47.8% in the placebo group.
- 89.5% of people with prediabetes in the STEP 3 trial and 89.8% in the STEP 4 trial returned to normoglycemia within 68 weeks of taking semaglutide.
- In a multi-country trial over 52 weeks, 81% of participants' blood sugar returned to normal levels after taking semaglutide, exercising regularly, and following a healthy diet.
Who is an Ideal Candidate for Pharmacological Prevention?
Since semaglutide is a prescription medication, a qualified healthcare provider must assess if it will be useful and if so, write a prescription. While this is determined on a case-by-case basis, there are some signs someone shouldn’t take semaglutide:
- A personal or family history of medullary thyroid carcinoma (MTC)
- A diagnosis of Multiple Endocrine Neoplasia Syndrome Type 2
- An established hypersensitivity to any form of semaglutide
- A desire to get pregnant or a current pregnancy
- An allergy to any inactive ingredients in Rybelsus, Wegovy, or Ozempic
Beyond the Pill: Integrating Lifestyle for Lasting Results
Semaglutide isn’t a standalone solution. For the best results, the FDA recommends taking this medication while implementing or maintaining healthy habits. For prediabetes specifically, focus on eating a healthy diet, working out, and regularly meeting with a healthcare provider.
The Anti-Inflammatory Power of a Balanced Diet
A balanced diet can help stabilize blood sugar levels, especially when it includes anti-inflammatory foods such as:
- Leafy greens
- A rainbow of fruits and veggies (i.e., fruits and veggies of many different colors)
- Lean proteins, like fish, tofu, and grilled chicken
- Nuts and seeds
- Healthy fats, such as those in avocado or olive oil
- Whole grains, like whole grain pasta or brown rice
- Legumes, such as chickpeas or lentils
The above food groups are associated with weight loss or healthy weight management, which may help reverse prediabetes. A low-calorie diet is also useful at reducing blood sugar spikes and for weight loss, so long as those calories come from anti-inflammatory foods and not overly processed options like chips, pastries, and fries.
Physical Activity: The Best Medicine for Insulin Resistance
A recent study found that exercising 150 minutes or more a week increased the likelihood of reversing prediabetes. That’s because regular workouts can help make cells more responsive to insulin. The body also absorbs glucagon during exercise, which lowers blood sugar levels as well. Plus, workouts can help manage weight.
Exercise doesn’t have to look like training for a marathon or becoming a bodybuilder. It could mean taking a 30-minute walk five days a week or doing a mix of yoga, strength training, and walking, totaling 150 minutes (or more) of weekly movement.
Regular Monitoring and Doctor-Patient Partnership
Regular appointments with a healthcare provider can help hold you accountable for lifestyle changes and allow your provider to keep track of any changes in blood sugar levels.
A healthcare provider may also advise you on if you should consider semaglutide to reverse prediabetes, additional lifestyle changes that may help, and any other treatment options that may be useful.
Taking Proactive Control: A Long-Term Health Perspective
Many people, but not everyone, who receive a prediabetes diagnosis will eventually be diagnosed with type 2 diabetes. To be one of the people who reverses this condition, it’s important to take control of your health and develop habits you can sustain in the long-term.
Moving from "At Risk" to "Healthy": A Mindset Shift
Navigating lifestyle changes and medication options for prediabetes is overwhelming. While your medical team can assist you, developing a mindset where you view yourself as someone who is actively and successfully building a healthy life also helps.
Ways to shift to that mindset include:
- Celebrate progress — you could even write a list of small prediabetes management wins, such as completing a workout or choosing a healthier snack option.
- Choose one or two big changes to implement at a time. Once you’re consistent with those, add in more.
- Learn more about what impacts blood sugar levels and effective ways to manage prediabetes.
- Lean on loved ones and possibly a mental healthcare provider for emotional support.
- Be kind to yourself throughout the process. Changes are easier when you appreciate how far you’ve come instead of beating yourself up over any setbacks.
Potential Side Effects and Safety Profile
If exploring semaglutide for prediabetes, assess any potential side effects. Semaglutide is safe for diverse patient populations and treatment durations, but it still has some side effects to be aware of:
- Anxiety
- Blurred vision
- Constipation
- Diarrhea
- Faster heartbeat
- Fatigue
- Fever
- Headaches
- Lightheadedness
- Nausea
- Shakiness or weakness
- Stomach pain
- Sweating
- Vomiting
- Yellow skin or eyes
In one study, about one third of patients reported some side effects, though many were manageable. If worried about semaglutide’s safety before taking it or while on the medication, discuss any concerns with the prescribing healthcare provider.
Semaglutide helps people to not only reverse prediabetes, but to lose weight, feel more energized in their day-to-day lives, and develop better overall health. When combined with lifestyle changes, you can also develop sustainable, consistent routines that allow you to feel healthier and happier for years to come.
Frequently Asked Questions

Expert-Guided, Sustainable Weight Loss
Discover how proven medications such as semaglutide or tirzepatide, combined with expert support, can help you reach lasting weight loss results.


 Medically Reviewed
Medically Reviewed



