Key Takeaways
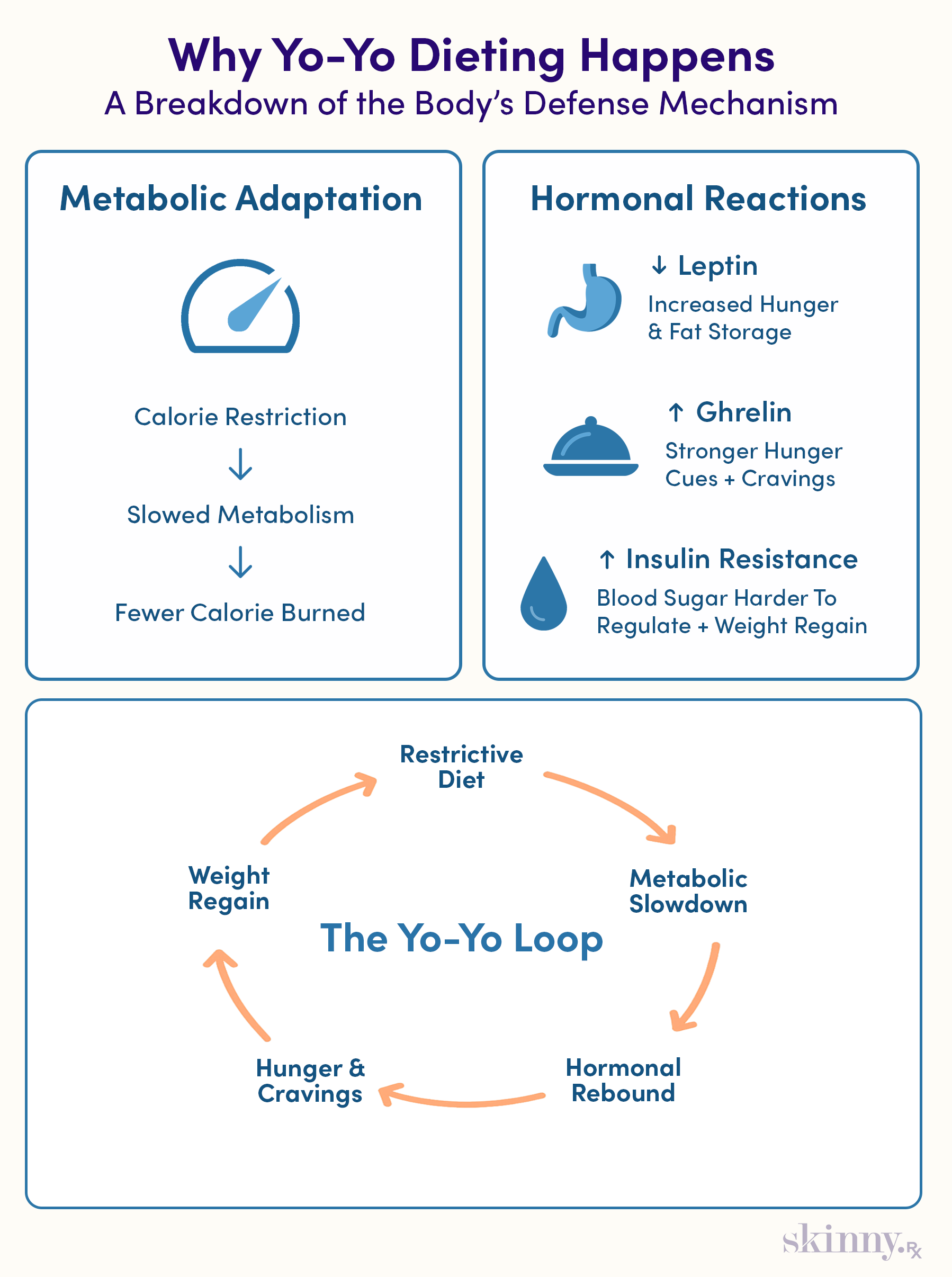
- Yo-yo dieting is driven by metabolic slowdown, psychological eating triggers, and restrictive diets that make long-term weight maintenance difficult.
- Dieting lowers metabolism and causes hormonal rebound. Leptin drops, ghrelin rises, and insulin resistance increases, which intensifies hunger and promotes weight regain.
- Semaglutide helps counter these biological drivers by reducing hunger signals, slowing gastric emptying, enhancing fullness, and supporting blood sugar stability.
- Many users experience less food noise and fewer cravings on semaglutide, which improves consistency with healthier eating and reduces the likelihood of rapid regain.
- Long-term results depend on sustainable habits. Balanced nutrition, mindful eating, regular exercise, and healthier mindset patterns help maintain weight during and after semaglutide.
From quick-fix diets to viral challenges like 75 hard, the weight loss industry often delivers ways to drop pounds fast. Keeping them off is another story. If the weight returns after a successful diet, the frustrating cycle of yo-yo dieting begins, and it’s a stubborn pattern to break.
“Yo-yo dieting is common among people who have been struggling to lose weight for years,” says Whitney Lisenmeyer, PhD, RD, an Assistant Professor of Nutrition and Dietetics at Saint Louis University, “Semaglutide may help not only with weight loss, but also help to break a pattern of yo-yo dieting and its related physical and emotional challenges.”
This weight loss medication quiets hunger signals, reduces food cravings, and stabilizes blood sugar, all of which make it easier to keep the pounds off and build a healthy lifestyle you can actually stick with. Here’s what you need to know about semaglutide and yo-yo dieting.

Yo-yo dieting is common among people who have been struggling to lose weight for years. Semaglutide may help not only with weight loss, but also help to break a pattern of yo-yo dieting and its related physical and emotional challenges.
–
Whitney Linsenmeyer, PhD, RD, Assistant Professor of Nutrition and Dietetics
The Frustrating Reality of Yo-Yo Dieting
Weight regain is quite common, with one study suggesting less than 6% of people sustain weight loss 15 years after undergoing a weight loss program. When someone regains the pounds quickly, sometimes within weeks or months, it’s referred to as yo-yo dieting or weight cycling.
What is Weight Cycling and Why Is It So Common?
Weight cycling, when someone goes back and forth between losing weight and regaining it, occurs when the body, brain, and even the diet itself work against sustainable weight loss:
- The body: Biologically, the body may slow metabolism and reduce total energy expenditure in response to fewer calories. That means even if someone eats less, they may not burn enough calories for significant weight loss. This effect can last years for some, even if calorie intake increases, making it hard to avoid weight regain.
- The brain: Psychologically, many people who are overweight or obese eat in response to negative feelings or thoughts or have binge eating tendencies. In either case, the brain is sending constant cues to eat, and this “food noise” can be difficult to manage when aiming to lose weight.
- The diet: If someone chooses a highly restrictive diet, such as the keto diet or a very low-carb diet, the guidelines are hard to stick to in the long run. This makes weight cycling even more likely when returning to one’s usual eating patterns.
The Physiological and Psychological Toll of Dieting Failure
You can think of yo-yo dieting like a roller coaster with extreme highs and lows. Just like a roller coaster upsets a motion-sensitive stomach, weight cycling can disrupt overall health. In fact, it slows metabolic processes, contributes to insulin resistance and increases the risk of heart disease and type 2 diabetes.
Difficult emotions, like depression and stress, accompany yo-yo dieting too. A rapidly changing body may bring up body image issues, and it’s difficult to come to terms with what may be perceived as “weight loss failures” when the number on the scale ticks back up.

Expert-Guided, Sustainable Weight Loss
Discover how proven medications such as semaglutide or tirzepatide, combined with expert support, can help you reach lasting weight loss results.
The Science Behind Weight Regain: Your Body's Defense Mechanisms
As we’ve alluded to, there are a few biological reasons for yo-yo dieting. Many relate back to metabolism, which is the body’s way of turning food into usable energy.
Metabolic Adaptation: Slower Metabolism, Increased Hunger Hormones
Once someone puts on weight, their body adjusts to the higher caloric intake. Calories are the fuel the body uses to power workouts, everyday activities, and even the bodily functions that keep us alive. Dieting means reducing caloric intake, and in turn, the body cuts back on its energy expenditure, aka slows metabolism.
This slowdown, however, may last years after someone finishes a diet, meaning metabolism remains slow even if caloric intake increases, potentially causing weight gain.
As soon as someone starts dieting, a few hormones also cue the brain to eat more in order to keep the caloric intake at the status quo:
- Leptin: Leptin is a hormone that helps tell the brain when the body is hungry and full. Levels decrease with weight loss, which may make the brain want to eat more. Lower levels also cue the body to store more fat, potentially contributing to weight regain.
- Ghrelin: Another hormone that sends hunger signals to the brain is ghrelin. When someone loses weight, ghrelin levels increase in an attempt to maintain the same caloric intake as before. This can make it harder to not eat more.
- Insulin: To help the body absorb carbohydrates from our diets, the pancreas creates insulin, a hormone that regulates blood sugar levels. Weight cycling, however, may increase insulin resistance, meaning this hormone isn't as effective at regulating blood sugar levels. Insulin resistance may contribute to long-term weight gain.
How Semaglutide Interrupts the Yo-Yo Cycle
Semaglutide is a weight loss medication that mimics a naturally occurring hormone, GLP-1. GLP-1, which effectively reduces hunger cues, slows gastric emptying, which can make someone feel full for longer, and works alongside insulin to lower blood sugar levels after a meal.
Addressing Metabolic Adaptation: Counteracting Hunger Signals
Semaglutide mimics GLP-1, a hormone that may counteract the increased hunger cues from ghrelin and leptin. Taking semaglutide may also result in greater fullness after eating and lower overall calorie intake.
All of these benefits may make it easier to stick to a healthier diet. Semaglutide also assists with insulin function, contributing to a more effective metabolization of blood sugar.
Enhancing Satiety and Reducing Food Cravings
Since semaglutide helps someone feel full for longer and decreases hunger cues, many people who take this drug report less food noise, obsessive thoughts about food, and fewer cravings for hyperpalatable food, like french fries or ice cream.
Beyond the Medication: Integrating Lifestyle for Lasting Success
While three forms of semaglutide are FDA-approved (Ozempic and Rybelsus for type 2 diabetes, and Wegovy for weight management), the FDA notes that these medications work best alongside lifestyle changes. Healthy habits to implement alongside semaglutide include mindful eating, diet changes, regular workouts, and mindset changes.
Mindful Eating: Cultivating a Healthier Relationship with Food
To cultivate a healthier relationship with food, look at what you eat and how you eat. On the what-you-eat front, prioritize foods that fuel you:
- Fiber can help you stay full for longer
- Sources of lean protein, like chicken or fish can help build muscle
- Fruits and veggies may lower overall caloric intake and decrease the risk of certain weight-related conditions, like heart disease.
Mindful eating is the practice of eating slowly and savoring each bite. It can help curb cravings and emotional eating. Mindful eating strategies include:
- Eating without distractions, such as social media or TV
- Chewing food completely before eating another bite
- Focusing on how food tastes, smells, looks, feels, and sounds when eating
- Putting utensils down between each bite
Consistent Physical Activity: Muscle Mass and Metabolic Health
150 minutes (minimum) of cardio each week may help you burn more calories than you eat. Cardio could look like a vigorous run or a more leisurely walk or bike ride. Strength training two or more times a week can help burn calories as well as build muscle mass.
Shifting Your Mindset: From Dieting to Sustainable Health
Yo-yo dieting has negative implications for mental health. To break the cycle, it’s important to make space for a healthier relationship with food and body image. Small steps toward a mindset shift include:
- Thinking more positively about yourself
- Speaking to yourself like you would a friend, especially when it comes to weight and what you eat
- Tracking progress toward eating healthy and exercising regularly
- Celebrating when you are consistent
Preparing for the Long Term: Sustaining Weight Loss After Semaglutide
Semaglutide isn’t a quick fix. It’s part of a long-term weight management plan. Sometimes that plan involves discontinuing the medication, and other times it’s a lifelong medication.
The Possibility of Continued Medication
Semaglutide is more than a weight loss drug. It also lowers the risk of diabetes-related chronic kidney disease, heart failure, cardiovascular disease, and non-alcoholic fatty liver disease. Plus, it helps with blood sugar regulation for individuals with type 2 diabetes.
If using the medication to reduce the risk of these conditions or as part of diabetes management, your doctor may advise you to continue with semaglutide, especially if not experiencing any major side effects. It is important to consult your doctor when starting, stopping, or changing any prescription medication.
Strategies for Transitioning Off Medication
Other people decide to transition off semaglutide once they hit their weight loss goals. While it is possible to sustain weight loss after stopping semaglutide, one study found two-thirds of those who discontinue regain the weight within one year.
Building Sustainable Habits
So what exactly did that one-third who didn’t regain the weight do differently? While the study didn’t mention the reason, other research suggests a healthy diet and lifestyle can help reduce the likelihood of rebound weight.
This emphasizes that semaglutide alone may not be enough to stop yo-yo dieting, but it creates an opportunity to quiet the “food noise,” build sustainable habits, and lose weight with more ease.

Expert-Guided, Sustainable Weight Loss
Discover how proven medications such as semaglutide or tirzepatide, combined with expert support, can help you reach lasting weight loss results.


 Medically Reviewed
Medically Reviewed



