Key Takeaways
- When semaglutide leaves your system, GLP-1 activity drops. Appetite, digestion speed, and blood sugar regulation return to baseline, often causing hunger and cravings to reappear.
- Up to two-thirds of people regain lost weight within a year of stopping semaglutide, largely due to hormonal and metabolic changes rather than willpower alone.
- Slowly reducing your dose, typically every 4 to 8 weeks or longer under medical supervision, gives your body time to adjust and helps preserve weight-loss progress.
- A balanced, high-protein diet, consistent exercise, quality sleep, and stress management are proven to counteract metabolic slowdown and prevent rebound weight gain.
- Working closely with your healthcare provider can help you customize your taper schedule, monitor blood sugar changes, and decide whether to continue on a low dose long term.
While semaglutide is effective and safe, not everyone needs to stay on it forever. Whether you’re stopping due to severe side effects or you’ve met your weight loss goal and are ready to manage your health without the drug, you may be wondering, “What happens when you stop semaglutide?”
There are some immediate side effects of stopping this medication, such as increased appetite and feeling hungry faster after a meal. Blood sugar levels may also return to what they were before taking the medication, and there is the potential to gain rebound weight.
Here’s everything you need to know about stopping semaglutide, as well as tips to successfully taper off this weight loss medication.
The Immediate Effects of Stopping Semaglutide
When you stop taking semaglutide, your body gradually loses the drug’s influence on the hormones that regulate blood sugar, digestion, and appetite. Semaglutide works by mimicking GLP-1, a naturally occurring hormone that triggers cell receptors in the digestive system and brain.
When activated—either by your body’s own GLP-1 or by semaglutide—these receptors do several things:
- Lower blood glucose or blood sugar levels after a meal
- Slow gastric emptying, meaning you feel full faster
- Reduce hunger cues and appetite
These three changes mean the drug can be an option to manage conditions related to blood glucose levels, like prediabetes and diabetes, and to help people lose weight.
It also means that after stopping semaglutide, the first impacts often relate to appetite and gastric emptying, as well as blood sugar levels.
The Return of Appetite and Cravings
Part of the reason semaglutide helps with weight loss is that it delays gastric emptying, meaning you feel full for longer on the drug. However, this delay can also lead to gastrointestinal (GI) side effects like nausea, abdominal pain, heartburn or acid reflux, constipation, and diarrhea. When you stop taking the medication, this delay goes away, with many reporting these GI symptoms do too.
Discontinuation also means that you may not feel full for as long after a meal, meaning it’s best to pay attention to nutrition and not overindulge cravings, which often return in full force soon after stopping the drug.
Changes in Blood Sugar
While semaglutide is famously touted as a “weight loss drug,” it can also help with blood sugar control, thanks to GLP-1’s role in regulating blood glucose levels. Once semaglutide is no longer in your system, blood sugar levels may rise to where they were before starting this medication. However, this is still an area being researched, with one study suggesting the improved glucose control remained after treatment for participants who took semaglutide for 68 weeks.
Should blood sugar levels increase, you may experience symptoms, such as:
- Feeling thirsty
- Headaches
- Feeling fatigued
- Urinating more often
- Blurred vision
If experiencing these symptoms after stopping semaglutide, contact a doctor for further evaluation. They may recommend another medication that can help manage blood glucose levels, such as Victoza (liraglutide) or Mounjaro (tirzepatide).
The Science of Weight Regain
Perhaps the most documented side effect of stopping semaglutide is weight regain, with a landmark study reporting that two-thirds of those who discontinue regain all the lost weight within one year.
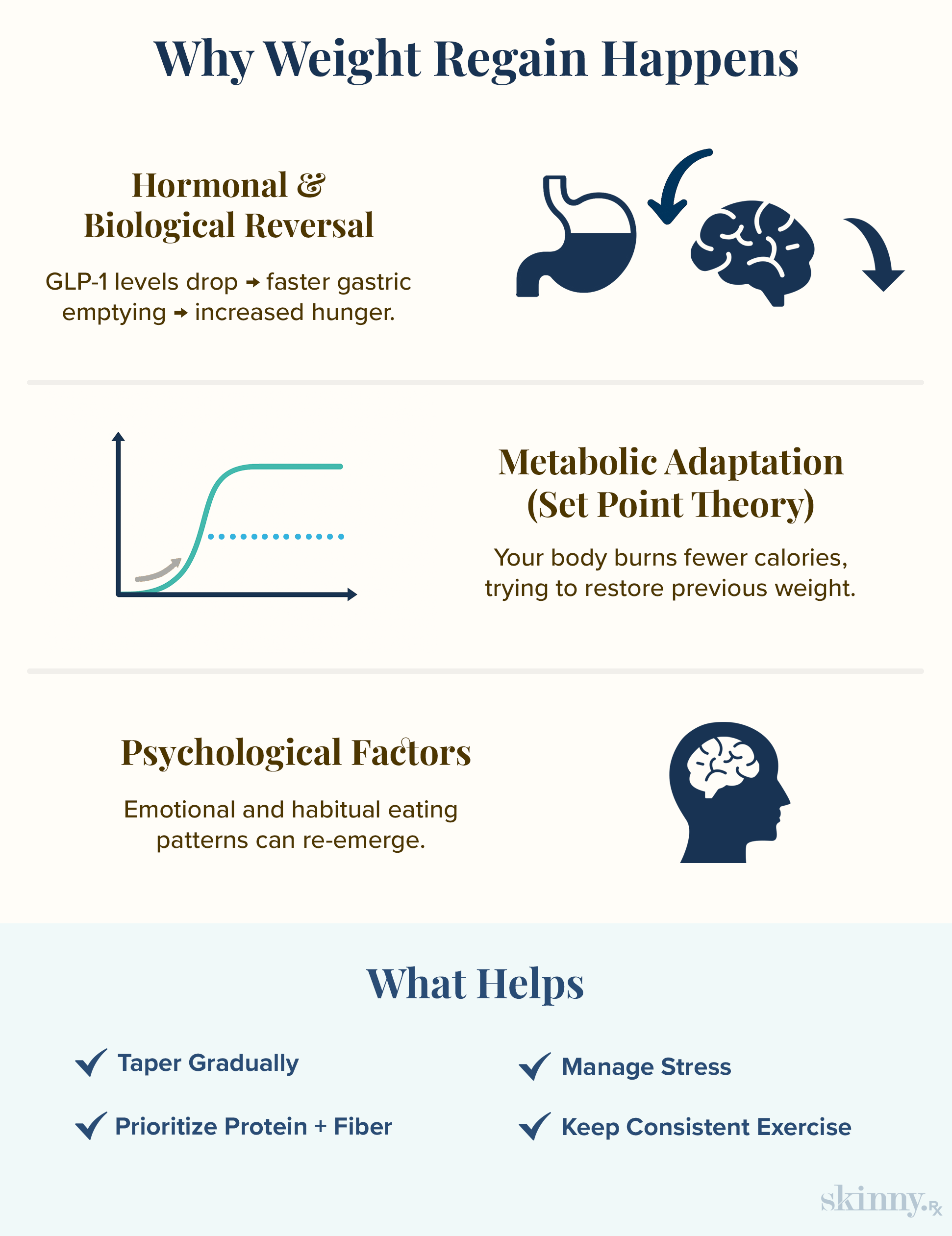
Hormonal Reversal (GLP-1's Absence)
Because GLP-1 promotes slower gastric emptying and helps curb hunger cues, people on this drug often eat fewer calories. This results in an average weight loss of about 15-25% in one year.
After stopping the drug, the body must rely on naturally occurring GLP-1, instead of that and semaglutide, which may mean faster gastric emptying and feeling hungrier after a meal. This may prompt people to eat more than necessary, increasing the likelihood of gaining weight.
Metabolic Adaptation and Set Point Theory
When someone takes semaglutide for a year or longer, they often experience a plateau where they stop losing weight. This plateau is referred to as a set point, which is where someone’s weight is in alignment with the ideal range determined by genetics and environment. Once you drop below that range, metabolism may actually slow in an attempt to move you closer to the set point.
That slow metabolism may remain after discontinuing semaglutide, and a slower metabolism makes it easier to gain weight as well as harder to lose weight in the future.
The Psychological Component
Emotional eating, when negative feelings like sadness, boredom, or anger act as a cue to eat in order to temporarily soothe negative emotions, is a common reason why someone may overindulge or eat more calories than they need. Semaglutide reduces “food noise,” obsessive thoughts about food that often trigger emotional eating, because of the drug’s impact on GLP-1 receptors in the brain.
When activated, these receptors reduce the food noise stemming from uncomfortable emotions. In one study, emotional eating dropped from 77.5% of participants before starting semaglutide to 11.5% after taking the medication.
When on these drugs, people report fewer cravings for hyperpalatable foods like chips, ice cream, and French fries, and less food noise. Once off these drugs, the noise and psychological cravings may reappear, making someone more likely to emotionally eat.
A Step-by-Step Transition Plan
While there are many potential effects of stopping semaglutide, many can be managed with the right treatment plan. At SkinnyFix, you can take a quick assessment to be paired with a licensed clinician who will guide you through a personalized tapering and maintenance plan designed to prevent rebound weight gain.
Tapering Your Dose
While you can safely stop semaglutide cold turkey, this may increase the chance of weight regain. Instead, slowly tapering off the medication may be more effective, especially if paired with guidance from a healthcare provider and lifestyle changes to maintain a healthy weight (which we’ll detail in the next section).
A gradual taper is often best, with some preliminary research suggesting to reduce the dose every four to eight weeks.
Plus, tapering provides more time to implement those lifestyle changes. “I have many patients who we will taper very slowly down on their medication dose, often only decreasing every 3 to 6 months,” says Daniel McGee, D.O., a board-certified family medicine physician, “This gives people more time to implement the habits and lifestyle changes needed to keep the weight off longterm.”

I have many patients who we will taper very slowly down on their medication dose, often only decreasing every 3 to 6 months. This gives people more time to implement the habits and lifestyle changes needed to keep the weight off longterm. If we need to stay on a low dose for a long time or increase temporarily to get back on track with weight loss goals, we can do that and monitor progress over the long term. This helps patients take the pressure off not feeling like they have to stop the medication quickly and can give them time to make new adjustments on their daily routine.
–
Dr. Daniel McGee, Board-certified Family Medicine Physician
Working with Your Healthcare Provider
A healthcare provider can help you determine the right tapering schedule and long-term weight maintenance plan. Questions to ask a healthcare provider when working with them on a taper plan include:
- How long of a taper would you recommend?
- How often should I reduce my dose?
- Are there any other medications or lifestyle choices I should make while tapering off semaglutide?
Depending on your reason for taking semaglutide, stopping without consulting a doctor may lead to adverse effects, such as high blood pressure. As a result, it’s not recommended to stop until you have the green light from your doctor.
Strategies for Long-Term Weight Maintenance
In the biggest study on discontinuing semaglutide, two-thirds of people regained all the weight within one year. While we don’t know exactly why the other third didn’t, a potential reason is that they had a long-term plan to keep the weight off. Other studies support this therapy, with a healthy diet and exercise being especially beneficial if trying to avoid rebound weight.
The Foundation: Diet and Nutrition
Semaglutide works best when paired with a healthy diet. Some food groups to add to your plate as you taper off are:
- Lean proteins, such as chicken, salmon, and tofu
- Healthy fats, like nuts, avocado, and olive oil
- High-fiber foods like chickpeas, lentils, and beans
- Complex carbs, such as quinoa, brown rice, and oats
- Plenty of fruits and vegetables
Since hunger cues may increase after stopping semaglutide, it may also be helpful to track your calories. The FDA has a tool that can help you determine how many you need based on age, gender, and activity level.
Exercise: Finding a Sustainable Routine
In one study, people who followed a one-year post-exercise program after stopping liraglutide, another GLP-1 medication that is similar to semaglutide, weren’t as likely to regain weight.
The program consisted of two instructor-led sessions with a mix of high-intensity cycling followed by circuit training, which builds muscle strength and endurance via exercises that utilize body weight or light dumbbells. The fitness instructors also encouraged participants to work out two times a week on their own.
A mix of strength training and cardio exercise (walking, cycling, jogging, etc.) may help maintain a healthy weight, whether you’re on semaglutide, stopping it, or have never taken this drug. Plus, attending instructor-led classes adds an element of accountability, making it easier to stick with exercise.
Lifestyle Factors: Sleep, Stress, and Support
While we often focus on diet and exercise when trying to lose weight, sleep deprivation and high stress levels can lead to weight gain as well.
Some quick ways to manage daily stress include:
- Take breaks from social media and the news
- Make time to unwind
- Engage in mindfulness practices like yoga, journaling, or meditation
- If short on time, try two to four minutes of 4-7-8 breathing
- Write a few things you’re grateful for each day in a notebook or the notes app in your phone
Practices that can increase the time you spend asleep and the quality of your sleep are:
- Have a set bedtime and time to wake up each day (even on weekends)
- Sleep in a cool, dark environment
- Avoid screens right before bed
- Engage in a calming activity before bedtime, like a warm bath or reading a book
- Avoid heavy meals, alcohol, and caffeine at least two hours before going to sleep
When to Consider Staying on Semaglutide
Semaglutide is an effective drug for many things, not just weight loss. Those on semaglutide have a lower risk of diabetes-related chronic kidney disease, heart failure, cardiovascular disease, and non-alcoholic fatty liver disease. Plus, this medication can play a role in blood sugar regulation for those with prediabetes or type 2 diabetes.
If tolerating the side effects of semaglutide and using it for type 2 diabetes or to lower the risk of medical conditions associated with being overweight or obese, it may make sense to stay on the medication. Those who have few side effects and are continuing to lose weight may also want to consider staying on this medication for longer.
If unsure if stopping or continuing is the right option, a healthcare provider may recommend a lower dose with the potential to taper off in the future. Dr. McGee explains, “If we need to stay on a low dose for a long time or increase temporarily to get back on track with weight loss goals, we can do that and monitor progress over the long term. This helps patients take the pressure off not feeling like they have to stop the medication quickly and can give them time to make new adjustments on their daily routine."

Expert-Guided, Sustainable Weight Loss
Discover how proven medications such as semaglutide or tirzepatide, combined with expert support, can help you reach lasting weight loss results.


 Medically Reviewed
Medically Reviewed



