Key Takeaways
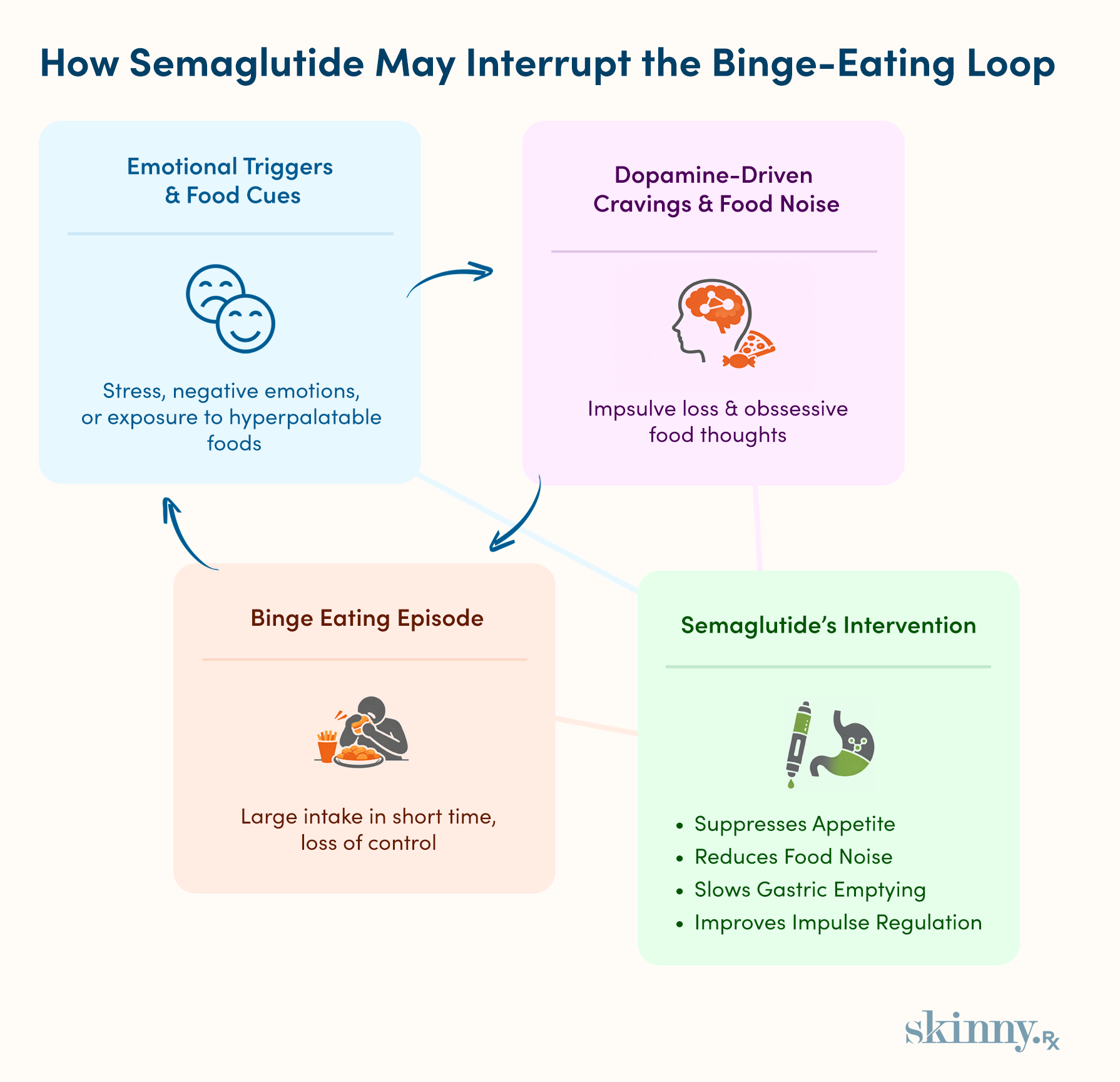
- Binge Eating Disorder is driven by emotional triggers, disrupted dopamine signaling, and impaired impulse control rather than hunger alone.
- Semaglutide may reduce binge urges by suppressing appetite, quieting food noise, and lowering cravings for hyperpalatable foods.
- Early studies show semaglutide can reduce binge frequency and severity, but findings are limited and not yet conclusive.
- Semaglutide is not FDA-approved for Binge Eating Disorder and is used off-label when considered.
- Medication works best when combined with psychotherapy and nutrition counseling to address emotional and behavioral drivers of binge eating.
Binge Eating Disorder (BED) is a serious psychological condition where someone eats large amounts of food in one sitting and can’t control what or how much they are eating. These episodes are often triggered by an emotion, like stress or feeling depressed.
Currently, there is one FDA-approved medication, Vyvanse, which helps with impulse control. However, emerging research suggests semaglutide may also be a useful tool to help treat BED.
Semaglutide reduces the intensity and frequency of food cravings, which may help with emotional eating and possibly binge eating. Here’s everything you need to know about semaglutide and binge eating, including when this pharmacological treatment for BED is a good idea.
Understanding the Complex Drivers of Binge Eating Disorder
Binge Eating Disorder (BED) is a psychological condition where someone eats large amounts of food, usually in a short amount of time. Often, the behavior is triggered by stress, negative feelings, or something bad happening in someone’s life. This cue creates an impulse to eat a lot of food quickly, with binges usually lasting less than two hours.
“Binge eating disorder is a complex condition that is driven by numerous factors within the body and the environment,” explains Whitney Lisenmeyer, PhD, RD, an Assistant Professor of Nutrition and Dietetics at Saint Louis University, “If you think you may have this condition, talk to your healthcare team about the range of treatment tools, which may include therapy, nutrition counseling, and medications."

Binge eating disorder is a complex condition that is driven by numerous factors within the body and the environment. If you think you may have this condition, talk to your healthcare team about the range of treatment tools, which may include therapy, nutrition counseling, and medications.
–
Whitney Linsenmeyer, PhD, RD Assistant Professor of Nutrition and Dietetics
Defining Binge Eating Disorder (BED): Diagnostic Criteria and Prevalence
To be diagnosed with binge eating disorder, someone must display at least three of the following criteria:
- Eating quickly
- Continuing to eat after someone is full, even if it’s uncomfortable
- Eating a lot of food, even if not hungry
- Eating alone, either most of the time or exclusively because someone is embarrassed to eat around others
- Feeling guilty, self-loathing, or disgusted after a binge eating episode
Three or more of those habits must occur once a week or more for at least three months in order to be diagnosed as BED. About 2.8% of Americans have experienced Binge Eating Disorder at some point during their life, and it’s more common in women than men.
The condition is similar to bulimia nerviosa, which is when someone binge eats and then compensates with vomiting, fasting, excessive exercise, or laxative or diuretic abuse. With Binge Eating Disorder, people do not compensate with these methods after a binge.
The Neurochemical Loop: Reward, Dopamine, and Compulsive Eating
There isn’t one known cause for Binge Eating Disorder. Psychological, social, genetic, and behavioral factors influence the likelihood of developing BED. That said, the condition works similarly to other substance abuse disorders, leading many to think that binge eating operates like an addiction.
When someone binge eats, the brain releases dopamine, a feel-good hormone. This effect can soothe stress or negative emotions, which are often a trigger for binge eating. Over time, binge eating becomes a coping mechanism in response to these triggers. There is some evidence as well that BED is associated with cravings for hyperpalatable foods, like cake, cookies, or fried foods. These foods may lead to a greater release of dopamine in the short term.
The Science of Control: How Semaglutide Intervenes
Currently, semaglutide is FDA-approved for weight management and type 2 diabetes, depending on the type of semaglutide. No types of semaglutide are FDA-approved for BED specifically. Yet semaglutide’s silencing effect on hunger cues and how it slows digestion may help with binge eating.
Dual Action: Suppressing Homeostatic and Hedonic Hunger
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist, meaning it mimics the effects of GLP-1, a naturally occurring hormone that helps control appetite. Semaglutide facilitates greater appetite suppression, meaning the urge to eat may not be as intense or frequent for those taking this drug.
The Brain Connection: Reducing "Food Noise" and Impulsivity
Binge eating is often related to food noise, or obsessive thoughts about food. This noise might look like constantly fantasizing about food, especially hyperpalatable options like pastries or hot dogs. These fantasies can interfere with the ability to complete everyday tasks or reduce impulse control to stop eating.
Disrupted hunger cues in the brain are responsible for food noise. Semaglutide activates receptors that help manage these cues, leading to better regulation. As a result, many people on the drug report less food noise and fewer cravings for hyperpalatable foods.
Gastric Effects: Slowing Digestion and Enhancing Physical Fullness
Whether naturally occurring or from semaglutide, GLP-1 slows gastric emptying, helping someone feel full for longer. When the stomach is physically full, stretch receptors send satiety signals to the brain, and this effect is associated with better eating control than before starting semaglutide.

Expert-Guided, Sustainable Weight Loss
Discover how proven medications such as semaglutide or tirzepatide, combined with expert support, can help you reach lasting weight loss results.
Emerging Evidence: Semaglutide's Effect on Binge-Related Behaviors
Semaglutide is a hot topic in the medical world, but few studies explore its potential impact on BED. That said, the existing research is promising.
Clinical Observations: Reductions in Episode Frequency and Severity
A landmark 2023 trial suggests that semaglutide may help treat binge eating disorder. In this trial, participants’ binge eating tendencies decreased by 14 points on the 46-point binge eating scale within three months of taking semaglutide. Similar studies with liraglutide and dulaglutide, two weight loss medications that work similarly to semaglutide, offered similar results.
A 2024 review on GLP-1 medications and binge eating suggested that semaglutide may decrease binge eating behaviors because of its effects on the receptors in the brain responsible for binge eating impulses.
However, that study also noted that research is limited. Plus, another 2023 article stated that in larger populations, semaglutide could either worsen or improve symptoms of eating disorders. Due to these mixed results, the National Eating Disorder Association states that while it’s possible semaglutide may help with binge eating disorder and bulimia nervosa, more research is required to confirm this possible benefit.
Impact on Cravings and Unwanted Food Thoughts
Where research is more conclusive is in how semaglutide reduces cravings and unwanted food noise. In a 2025 study, participants reported fewer food cravings after taking semaglutide, especially for carbohydrates or sugar. They also reported any remaining cravings were less intense, making them easier to resist.
Semaglutide’s reduction of food noise isn’t just a short-term effect either. Another study found participants on semaglutide could better control their eating habits for two years, meaning the drug could be a long-term solution.
A Multidisciplinary Approach: Integrating Medication and Therapy
If a healthcare provider prescribes semaglutide for binge eating disorder, know that it’s not a solo act. Semaglutide is a tool to manage the physiological urge, which creates space for psychotherapy to address underlying emotional triggers.
The Non-Negotiable Role of Psychotherapy (CBT and DBT)
Psychotherapy, often referred to as talk therapy, plays a crucial role in BED treatment. It helps individuals unpack the emotional triggers for binge eating and how their relationship with different feelings, like depression or stress, may lead to binge eating.
There are multiple therapeutic approaches that can help with BED. Some of the most evidence-backed include:
- Cognitive behavioral therapy (CBT): CBT is a common therapeutic style that addresses how someone's thoughts and feelings influence their behavior, as well as how they can positively change all three. There is strong evidence to support CBT’s role in treating binge eating disorders.
- Dialectical behavior therapy (DBT): This therapeutic approach focuses on teaching people skills and coping mechanisms to deal with difficult emotions in a healthier way. It also improves relationships, such as to food in the case of binge eating. DBT leads to similar behavioral changes as CBT, making it another great choice for treating binge eating.
- Interpersonal psychotherapy (IPT): This approach is commonly used for bulimia nervosa, though it may be useful for BED as well. IPT focuses on relationships or societal influences that cause unwanted behaviors, feelings, or perceptions of someone’s own body.
Nutritional Counseling: Repairing the Relationship with Food
In therapy, people can explore their relationship with food. Nutrition counseling helps develop the eating habits to support that new and improved view on food. To make sure that someone’s diet supports a healthier relationship with food, many people with BED undergo nutritional counseling with a registered dietitian.
Safety, Side Effects, and Setting Realistic Expectations
Just like any drug, semaglutide comes with side effects. It also doesn’t work overnight—semaglutide takes time to deliver results. Some people experience results in the first four weeks, though semaglutide’s effects often improve when someone takes the medication for a year or longer.
And keep in mind that most studies report on results related to weight loss or blood sugar control—the evidence is mixed if semaglutide helps with binge eating.
Potential Side Effects of Semaglutide
Semaglutide may cause side effects. The most common are:
- Nausea, potentially with vomiting
- Pain in the stomach
- Runny nose
- Sore throat
- Constipation
- Burping
- Headache
In rare cases, the medication may result in more severe side effects:
- Changes in vision
- Ongoing, severe stomach pain
- Rash
- Fainting
- Swelling in feet, legs, or ankles
- Yellowing of skin or eyes
- Pounding or quick heartbeat
- Severe gastrointestinal side effects
Most people can tolerate the drug’s side effects, and the severe ones are uncommon. If on the medication and experiencing side effects that cause discomfort or interfere with daily life, talk with a prescribing healthcare provider. They can offer ways to manage side effects or offer semaglutide alternatives.
The Importance of Ongoing Medical and Psychological Support
When using semaglutide, it’s important for a healthcare provider to regularly monitor progress. If using this medication to help with binge eating, someone may also benefit from regular check-ins with a therapist, who can help them redefine their relationship to food and explore BED’s emotional triggers.
If cravings or binge eating feel hard to manage, you can take a short assessment with us at SkinnyRx to explore doctor-prescribed weight loss options like semaglutide. Each assessment is reviewed by a licensed medical provider to help guide safe, individualized next steps.


 Medically Reviewed
Medically Reviewed



