Key Takeaways
- Total calories still matter most. Fasting helps reduce intake by shortening your eating window, but overeating within that window can cancel out your deficit.
- Fasting while on semaglutide can enhance fat loss, but the combination may increase your risk of muscle loss, fatigue, or digestive discomfort, especially if you’re under-eating.
- A 12-hour fast is a good entry point. If you feel good, you can work up to 16:8 or 18:6 windows as long as you’re not pushing through fatigue or nausea.
- Hit your daily protein target—between 0.7 and 1 gram per pound of body weight—to help you preserve muscle mass and strength levels.
- Pay attention to side effects. If fasting worsens your symptoms or impacts your workouts, recovery, or day-to-day function, it’s okay to stop. You don’t have to fast to make progress.
- Consult a doctor. If you're unsure whether fasting is right for you while on semaglutide, talk to your doctor or a registered dietitian who understands GLP-1s.
Intermittent fasting is a popular way to lose weight and keep it off. Pairing semaglutide and IF—a strategy restricting your eating to a specific time window—might accelerate fat loss by creating a caloric deficit. But there are risks to consider.
Many people wonder if intermittent fasting on semaglutide (brand names: Wegovy®, Ozempic®) can be done safely and effectively. The short answer: yes, but with a few important caveats.
Here’s what to know before you pair the two, and how to fast smart without sacrificing energy and strength.
The Benefits of Combining Semaglutide and Intermittent Fasting
Faster Weight Loss
People who follow intermittent fasting protocols often see reductions in total weight, body fat, and waist circumference. But despite what some fitness influencers may say, there’s no magic in skipping breakfast.
Calories still matter most for weight change. So fasting in and of itself isn’t some miracle method that burns fat; it’s a way of controlling your caloric intake by shortening your eating window. With less time to eat, most people naturally consume fewer calories—about 300 fewer per day, according to one study on eight-hour time-restricted eating.
For context, one pound of fat equals roughly 3,500 calories. To lose a pound per week, you’d need to maintain a daily deficit of around 500 calories. No studies have specifically looked at intermittent fasting and semaglutide, but scientists recognize we need more research in this area. That said, following intermittent fasting may be easier with a GLP-1 agonist like Wegovy® since these medications can help to suppress your appetite.
Improved Insulin Sensitivity
Insulin is a hormone that shuttles sugar into your cells for energy or storage as fat. Eating carbohydrate-rich foods causes your blood sugar to rise, resulting in a spike in your insulin and possible food cravings post-spike.
Fasting allows your blood sugar levels to even out by relying on carbohydrate and fat stores for energy. Multiple studies have been conducted on people with type 2 diabetes (and pre-diabetes) to assess how restricted eating windows affect blood sugar.
One article, published in Frontiers in Nutrition, concluded that time-restricted eating may result in weight loss and improvements in insulin sensitivity in those with diabetes. And a five-week study on men with prediabetes found that eating within a six-hour window improved insulin sensitivity and reduced fasting insulin levels.
So, does fasting make semaglutide more effective? Research is needed to explore how these two approaches interplay, but the appetite-suppressing and insulin-regulating effects may work in tandem.
Simpler Meal Planning
Fasting potentially curbs your food intake by narrowing your eating window and semaglutide limits your hunger and cravings. Combine the two, and you’ll likely find yourself eating fewer meals, which means fewer dishes and less time in the kitchen.
If you usually spend 15 minutes making breakfast each morning, skipping that one meal saves you nearly two hours per week. That’s two extra hours you could spend working out, relaxing, or finally learning to juggle. You’ll also presumably save some money as you only need to buy enough groceries for two meals plus some snacks. That’s another underappreciated bonus of fasting long-term.

A Smarter Path to Sustainable Weight Loss
Sustainable weight loss isn’t about doing more. It’s about doing what works. Explore a medically guided GLP-1 program designed for precision and long-term success.
Risks and Challenges
Potentially More Muscle Loss
A steep caloric deficit can lead to muscle loss. Since GLP-1 agonists already curb hunger and promote caloric restriction, you’ll want to watch how much you’re eating. If you find yourself way under-eating during your fasting windows, try adding in a meal or a snack or two.
The key to preventing muscle loss on semaglutide and IF lies in a combination of strength training and adequate daily protein and energy intake. Strength training while on semaglutide is crucial to preserving your muscle mass. It’s a way to signal to your body, “hey, I’m using this muscle, so let’s keep it around, please.”
Worsened GI Side Effects
Semaglutide can cause nausea, constipation, and diarrhea, which are unpleasant at best. (Excessive burping on semaglutide is also a GI-related side effect, which isn’t likely as debilitating.) At worst, these side effects can disrupt your workouts and lead to dehydration. The research on fasting and gut health is still evolving, with mixed results.
One article showed that short-term fasting may reduce heartburn and acid reflux, while mainstream publications report digestive issues as a potential side effect of fasting. If you feel like your stomach is on the fritz, there may be a couple of reasons why:
- General changes in diet, like the amount of food you eat, can impact gut health.
- Also, if you eat a larger-than-normal meal, which you’re prone to doing after not eating for many hours, you may upset your stomach.
How you feel while fasting is personal. Some individuals report that semaglutide nausea gets worse with fasting, and some don’t. Pay attention to your stomach during and after your fasting window, and adjust as needed. Always consult a doctor if symptoms persist.
Energy Crashes
If you’re new to both, be mindful of semaglutide fasting blood sugar concerns, especially in the first few weeks when your body is adapting. It’s not unusual to feel sluggish when you first start fasting. With fewer meals, your blood sugar may dip, leading to temporary fatigue or even brain fog until your body adapts.
As food intake becomes less frequent, your body begins tapping into its glycogen (carbohydrate) and fat stores for energy. Eventually, it shifts to burning stored fat, but that transition takes some time. And even once you’ve adapted, a simple truth remains: consuming less energy can mean having less to expend. So yes, feeling a bit tired early on is normal.
When to Stop Fasting
If fasting makes daily movement, work, or workouts harder than they should be, it may not be the right fit, at least for now. If you’re considering multi-day fasts, talk to your doctor first. There are still unknowns around semaglutide and prolonged fasting risks.
Fasting is just one strategy for managing your calorie intake, and like any approach, it can have downsides. Combine fasting with semaglutide, and you do run the risk of limiting your food intake too aggressively. Listen to your body and adjust as needed. You don’t have to fast to progress; it’s simply one option that may work well for some but not everyone.

Intermittent fasting and semaglutide both come with possible benefits and risks. Consult your healthcare team before starting any new diet, especially if you are managing multiple conditions.
–
Whitney Linsenmeyer, PhD, RD, Assistant Professor of Nutrition and Dietetics
How to Combine Semaglutide and Intermittent Fasting Safely
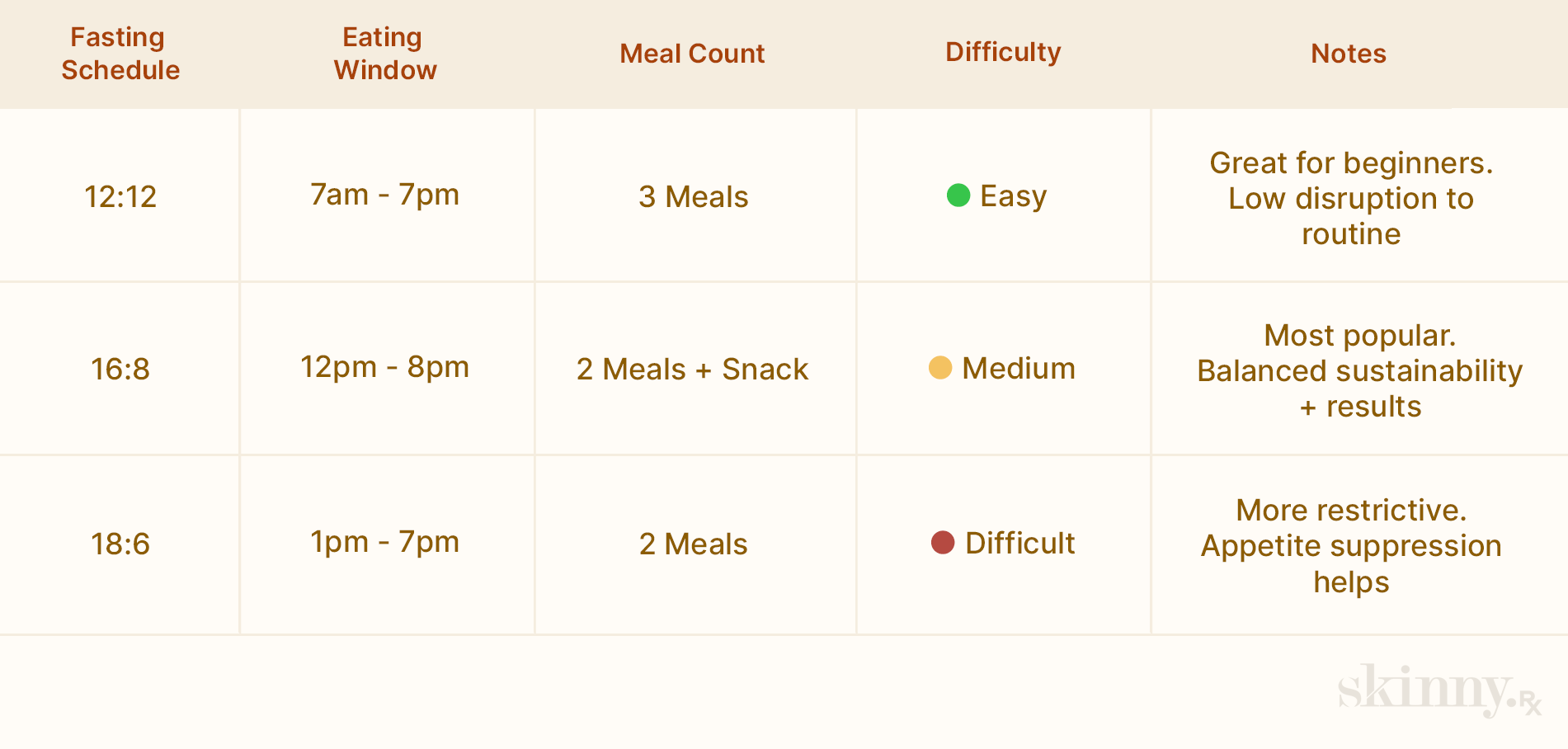
Here’s how different fasting windows stack up, plus how semaglutide might change how each one feels.
Choose a Fasting Window
There are many ways to approach fasting. Some people go a full 24 hours without eating once or twice a week, but a common method is daily time-restricted eating. That is, limiting food intake to a set window, like eight hours.
Fasting can help reduce calorie intake by shortening the time you have to eat. But at the end of the day, total calories still matter most. You could fast for 18 hours and still gain weight if your meals are consistently oversized or packed with high-calorie foods. On the flip side, eating balanced meals, centered around protein, vegetables, and complex carbs, even within a moderate fasting window, can support weight loss.
With that in mind, here’s a simple intermittent fasting schedule for semaglutide beginners that eases you into longer fasting windows.
- 12-Hour Fasting Window (12:12) (Example: 7:00 a.m. to 7:00 p.m.): This is a good entry-level window for fasting beginners. Most people already eat within a 12-hour window without realizing it, but committing to this structure can help curb late-night snacking and instill a sense of boundaries without feeling overly restrictive. Think of it as “fasting-lite”—a solid way to build discipline and consistency.
- 16-Hour Fasting Window (16:8) (Example: 12:00 p.m. to 8:00 p.m.): This is the sweet spot for intermittent fasting. You’ll skip breakfast but still have time for lunch, dinner, and a snack or two (depending on your hunger levels). While there’s no universal answer, many consider 16:8 the best fasting window for Ozempic® users because it strikes a balance between calorie control and long-term sustainability.
- 18-Hour Fasting Window (18:6) (Example: 1:00 p.m. to 7:00 p.m.): This is fasting on hard mode. With only six hours to eat, you’ll likely default to two meals and maybe a snack, making it easier to stay in a calorie deficit. Hunger may be more noticeable, especially early on, but semaglutide and other GLP-1 medications can make this approach surprisingly doable.
Critical Nutrients to Prioritize
Nutrients are the chemical compounds your body relies on to support essential functions like tissue repair, vitamin storage, and muscle growth. If you're taking a medication or following an eating protocol that puts you in a significant calorie deficit, it’s imperative to stay mindful of your nutrient intake.
Falling short on key nutrients can lead to muscle loss, fatigue, and brain fog—all things that work against your goals.
Here’s a brief breakdown of the key nutrients you should be aware of when fasting on semaglutide:
Disclaimer: Always consult with your doctor before starting a new medication or diet change, and if you’re concerned about a potential nutrient deficiency.
Protein
Protein is one of the three essential macronutrients (alongside carbohydrates and fats). It's critical for muscle maintenance, hormone production, immune function, and tissue repair. We’re calling it out here because adequate protein intake coupled with resistance training is the most effective way to preserve lean muscle mass while in a calorie deficit, which is almost guaranteed when combining semaglutide with intermittent fasting.
Aim for 1.6–2.0 grams of protein per kilogram of body weight per day (or roughly 0.7–1 gram per pound).
Carbohydrates
Carbs are your body’s preferred energy source. When digested, they’re converted into glucose to fuel your brain, muscles, and metabolism. While low-carb diets can be effective for some, cutting carbs too aggressively, especially while on a GLP-1 like semaglutide, can lead to fatigue, poor recovery, and digestive issues.
To maintain energy and support gut health, focus on whole-food carbohydrate sources like potatoes, oats, fruit, rice, legumes, and fiber-rich vegetables.
Electrolytes
Electrolytes—primarily sodium, potassium, and magnesium—are minerals that regulate hydration, muscle contractions, nerve function, and pH balance. Most people can take in adequate electrolytes through their normal diet. But, if you are sweating heavily (or experiencing gut symptoms like diarrhea), supplementing with electrolytes for fasting on GLP-1 agonists is especially important, as semaglutide can increase the risk of dehydration due to nausea or low food volume.
Consider using an electrolyte supplement like LMNT or Liquid I.V., especially during longer fasts or hot weather. Most are safe for healthy individuals, and the body typically excretes excess minerals.
Fiber
Since constipation is one of the most common side effects of semaglutide, fiber is a critical nutrient to supporting regular gut health. Plus, soluble fiber—the kind found in many fruits, vegetables, and other plant foods—will also help to control blood sugar levels.
Focus on fiber-rich foods like beans, legumes, whole grains, nuts, seeds, vegetables, and fruits.
Vitamin B12
Though not a direct effect of fasting, low Vitamin B12 levels can occur with reduced overall food intake or long-term use of certain medications (including metformin, which is sometimes co-prescribed with semaglutide). B12 deficiency can lead to fatigue, cognitive fog, and nerve issues.
If you're consistently eating less, consider a B12 supplement or ensure your diet includes sources like fish, shellfish, eggs, dairy, meat, or fortified foods.
Hydration Strategies
GLP-1 medications can blunt your hunger and thirst cues, making it easy to forget to drink liquids. And when you eat less, you also consume less water-rich food (like fruits, veggies, and soups), which can lead to dehydration. Dehydration can manifest as fatigue, dizziness, constipation, and headaches. Here are some simple tips for staying hydrated:
- Start your day with water: Aim for a tall glass of water (16 ounces) 30 minutes of waking up.
- Set a timer: You may not feel thirsty, but regular sips throughout the day matter more than chugging once or twice.
- Add electrolytes: If you're fasting for long stretches or experiencing GI side effects from semaglutide, consider using a no-sugar electrolyte supplement like LMNT, Nuun, or Liquid I.V. (and you can opt for the sugar-free versions of these supplements if available)
- Monitor your pee: If your pee is a light yellow color, you’re all good. Dark yellow pee is a sign that you need to drink up.

A Smarter Path to Sustainable Weight Loss
Sustainable weight loss isn’t about doing more. It’s about doing what works. Explore a medically guided GLP-1 program designed for precision and long-term success.
Sample 16:8 Fasting Schedule (With Semaglutide)
Going 16 hours without food sounds tough until you realize you’ll be asleep for about half of it. That’s the beauty of the 16:8 intermittent fasting schedule: you fast for 16 hours, eat within an 8-hour window, and let your body handle the rest.
Below is a sample day of eating that offers roughly 2,000 calories and 140-ish grams of protein, which is enough to support muscle maintenance even in a calorie-restricted state. Of course, how many calories you need to lose weight (or maintain) depends on a variety of factors like your gender, age, height, weight, and activity level.
Disclaimer: The following meal plan is an example. Always consult with your doctor or a registered dietitian before making changes to your diet, especially if you’re managing a health condition or taking medication like semaglutide.
7:00–11:00 a.m. — Wake up
- Stick to calorie-free drinks like water, black coffee, or tea. Staying hydrated will help curb your hunger.
12:00 p.m. — Meal 1
- 2 eggs scrambled with vegetables (e.g., spinach, bell peppers, and red onion)
- 3 slices of turkey bacon
- 2 slices whole-grain sourdough toast with butter
2:00 p.m. — Snack
- A protein bar, Greek yogurt, or a serving of jerky
4:00 p.m. — Meal 2
- 6 oz teriyaki grilled chicken
- 1 cup brown rice
- Stir-fry veggies (e.g., carrots, snap peas, broccoli)
7:30 p.m. — Meal 3
- Cheeseburger: 5 oz 93% lean beef burger, whole grain bun, and 1 slice of cheddar cheese
- Side salad with light dressing of choice
- 1 cookie for dessert (yes, you can still have treats)
8:00 p.m. — Eating window ends
- Continue to drink water as desired.
Final Thoughts
Combining semaglutide with intermittent fasting isn’t for everyone, but the combo can be a powerful way to control appetite, reduce caloric intake, and accelerate fat loss. The key is to approach the pairing with intention. Start with manageable fasting windows. Prioritize protein, hydration, and whole foods. Pay attention to how your body responds, and don’t push through nausea, fatigue, or digestive issues just to stick to a clock.
Intermittent fasting is a method, not a mandate. If it helps simplify your day and improve consistency, great. If it makes your life harder, skip it.
At SkinnyRx, we provide medically supervised access to compounded GLP-1 medications like semaglutide and tirzepatide. Take a brief assessment to see if one of these options fits your goals.


 Medically Reviewed
Medically Reviewed



