Key Takeaways
- Fiber and semaglutide both slow digestion, creating a synergistic effect for fullness, blood sugar stability, and weight loss.
- Soluble fiber helps control appetite and glucose, while insoluble fiber supports digestion and regularity.
- Introduce fiber gradually (+5 g/day) with plenty of water to minimize bloating and discomfort.
- Overdoing fiber supplements or neglecting hydration can worsen constipation, diarrhea, or dehydration.
- Combining fiber with semaglutide can help reduce “food noise” and improve meal satisfaction.
Semaglutide is one of the most effective medications for weight loss available today. In clinical studies, people have lost up to 14.9% of their body weight after 68 weeks on Wegovy®. But if you’re not getting enough fiber, you might not be getting the full benefit.
Fiber plays a surprisingly essential role in supporting gut health, curbing semaglutide side effects like nausea and constipation. At the same time, it boosts satiety (fullness), helping you eat less during the day and lose more weight.
Below, we break down how fiber and semaglutide work together, and share expert tips for using fiber to accelerate results on weight loss medications like Ozempic® or Wegovy®.
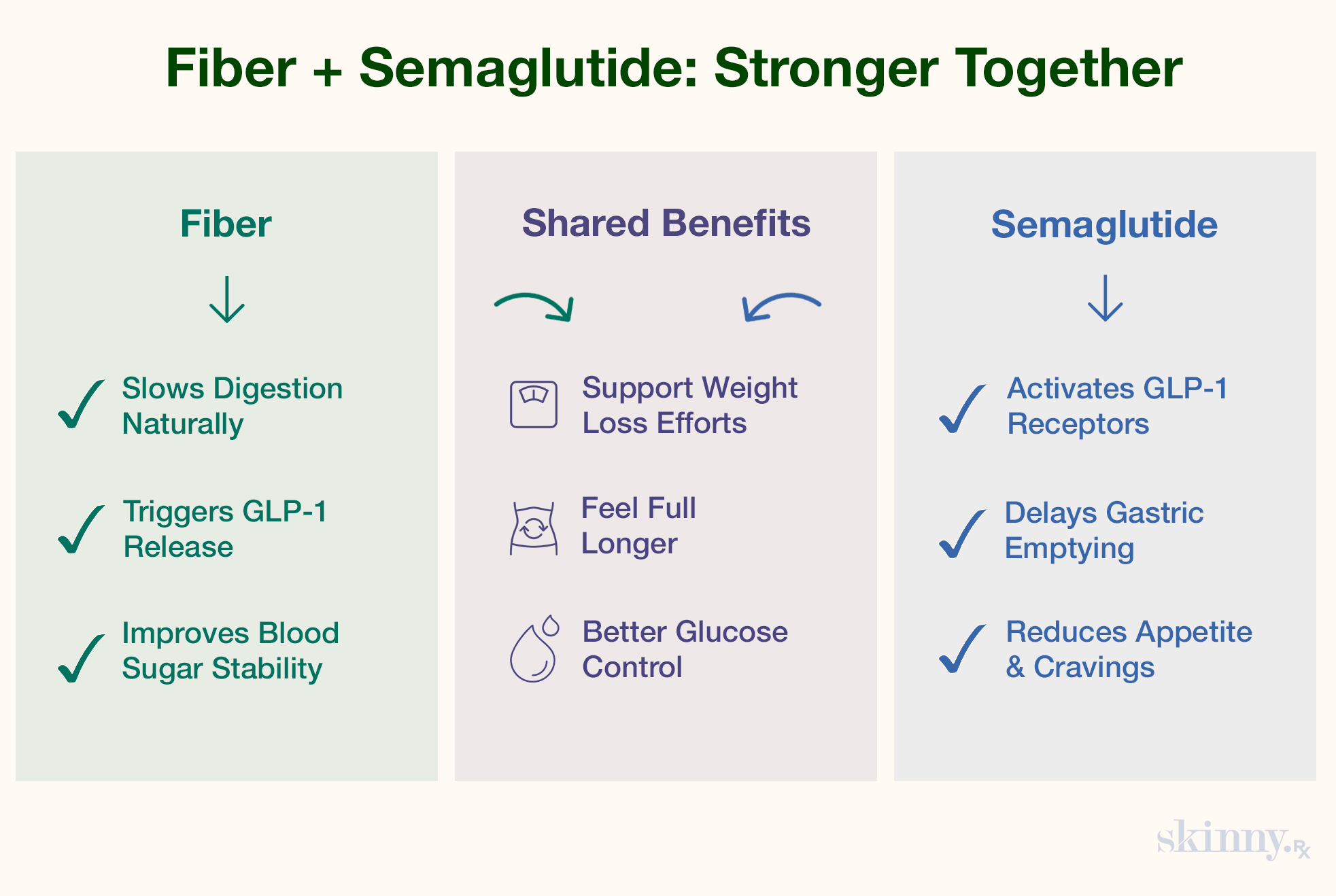
The Science of Fiber and Semaglutide Synergy
Semaglutide and fiber go together like, well, peanut butter and jelly (peanut butter, coincidentally, contains a decent amount of fiber). Fiber works so well with medications like Ozempic® or Wegovy® because it slows down digestion, just like semaglutide. And, fermentable fibers — like the kind you find in oats and legumes — may help encourage the release of GLP-1, the gut hormone that semaglutide mimics. Let’s take a closer look at how these effects work together.
How Fiber Enhances GLP-1’s Natural Effects
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist. This class of drugs treats obesity, type 2 diabetes, and other conditions by mimicking your body’s natural GLP-1 hormone to reduce appetite, slow down digestion, and stabilize blood sugar.
Dietary fiber has similar effects. When you eat high-fiber foods — including grains, avocados, legumes, raspberries, and nuts — your body releases more GLP-1 hormones. As a result, consuming fiber leads to many of the same effects that taking semaglutide does, including:
- Better blood sugar control
- Increased feelings of fullness
- Reduced appetite and food intake
In short, eating a healthy amount of fiber while taking semaglutide can help you eat less food, prevent blood sugar spikes, and lose more weight than relying on fiber or semaglutide alone.
The Role of Fiber and Semaglutide in Slowing Gastric Emptying
One of semaglutide’s key mechanisms of action is a delay in gastric emptying — that is, how quickly food leaves your stomach. This helps you feel full both sooner and longer, reducing your caloric intake and causing weight loss.
Fiber does the same. Fiber-rich foods (such as oats, lentils, and broccoli) absorb water and form a gel-like substance that slows digestion, making it an excellent match for semaglutide’s mechanism of action.
Together, semaglutide and fiber produce a longer-lasting feeling of fullness, which can help reduce cravings and “food noise.”
Fiber’s Benefits for Semaglutide Users
Eating a fiber-rich diet while taking semaglutide offers several benefits.
Fewer Side Effects, Including Constipation Relief
Constipation is one of the most common side effects of semaglutide, affecting as many as 12% to 35% of people on Ozempic® or Wegovy®. Thankfully, fiber is one of the best remedies.
Insoluble fiber nudges stool along your digestive tract, speeding transit. Paired with insoluble fiber, bulk-forming soluble fibers like psyllium husk support regular bowel movements, while soluble fiber softens stool to make it easier to pass. Ensuring you eat enough fiber, paired with generous adequate hydration (ideally from water or sugar-free liquids), can help relieve this uncomfortable side effect for those on semaglutide.
Appetite Control: Increased Satiety and Less “Food Noise”
People on semaglutide often describe a reduction in "food noise" — e.g. constant rumination about what you’ll eat next, or whether what you just ate was healthy.
Fiber can also quiet food noise and cravings by increasing satiety. When you eat fiber-rich foods, the fiber expands in your stomach, literally filling you up, while GLP-1 binds to receptors in the vagus nerve and brain to activate satiety (feeling full) pathways that curb appetite.
When you combine a fiber-rich diet with semaglutide, your meals can be smaller and simpler (e.g. containing more whole foods vs. processed ones), while still keeping you satisfied.
More Stable Blood Sugar Levels
Soluble fiber (like the glucomannan in oats and psyllium husk) helps regulate blood sugar by slowing the absorption of glucose. This not only complements semaglutide’s blood-sugar-lowering effects but also reduces the kind of blood sugar spikes and crashes that can lead to cravings.
That makes fiber a smart choice for people using semaglutide for weight loss, as well as those taking Ozempic®, Wegovy®, or compounded semaglutide to manage both their weight and type 2 diabetes.
Best Fiber Sources on Semaglutide
Fiber-rich foods are a healthy choice for weight loss in general, since they come from plant-based whole foods like grains, fruits, and vegetables. When you’re on semaglutide, it’s a good idea to incorporate both types of fiber — soluble and insoluble — into your diet.
Soluble vs. Insoluble Fiber: What’s the Difference?
Soluble fiber absorbs water while you eat, turning into a gel that slows down digestion.
Examples:
- Oats
- Barley
- Nuts
- Seeds
- Beans
- Lentils
- Peas
- Apples
- Pears
- Citrus fruits
- Carrots
- Broccoli
- Celery
- Cucumbers
Insoluble fiber accelerates digestion and bulks up your stool.
Examples:
- Wheat
- Whole grains
- Nuts
- Beans
- Barley
- Root vegetables
Soluble Fiber
Soluble fiber is your go-to for appetite control and blood sugar stability. Try eating it at the start of your day or before meals to slow digestion and boost satiety sooner. For example, you could have:
- Oatmeal with chia seeds in the morning
- A spoonful of psyllium husk in water before lunch
- Apple slices with almond butter as an afternoon snack (peanut butter can be a bit too fatty, potentially worsening side effects like nausea)
Insoluble Fiber
Insoluble fiber keeps things moving through your digestive tract, which is important since semaglutide slows everything down. Enjoy these fiber sources later in the day or after meals to aid motility:
- Brown rice or farro with dinner
- Roasted Brussels sprouts or carrots
- Popcorn (air-popped) as a light snack
Avoid overdoing it with raw cruciferous veggies (like broccoli) if you're prone to semaglutide side effects like bloating or abdominal pain. These foods have fermentable oligosaccharides, which can worsen GI symptoms.
Fiber Supplements
If your diet is low in fiber, or you’re experiencing ongoing constipation or nausea, fiber supplements can help. Psyllium husk and glucomannan are gentle, effective options.
Start with small doses and ramp up gradually to avoid gas or bloating. Reach out to your healthcare provider for more personalized advice.
Getting Started with Fiber on Semaglutide
By now, hopefully you’re super excited to start incorporating more fiber into your diet. Here are a few tips to ease the transition — especially if you haven’t historically eaten a ton of fiber — and set you up for weight loss success.
Week 1–2: Balancing Semaglutide Side Effects with Diet
In the first two weeks, you will likely be adjusting to the drug’s effects as semaglutide starts working in your body. When you’re being rocked by side effects like nausea, diarrhea, and potentially vomiting, this isn’t the time to dive in headfirst to 20+ grams of fiber.
Instead, start with an extra 5 grams of fiber per day and increase slowly. Focus on soluble fibers that are easy on your system first (like oats and apples) and drink at least 8–10 cups of water daily to help move it through your system.
Week 3–4: Adjusting for Optimal Digestion
Once your body has adjusted a bit to semaglutide, mix in more insoluble fiber. Notice how your body responds. If bloating or gas increase, scale back and add a digestive aid like ginger or peppermint tea.
Common Fiber Mistakes on GLP-1s
Considering that over 90% of Americans don’t meet the daily recommended guidelines for fiber intake, eating more fiber is generally a good idea. And, fiber can be particularly helpful for people taking semaglutide, considering its impacts on blood sugar and appetite. Having said that, there are some ways you can go wrong when boosting your fiber intake on semaglutide and other GLP-1s.
Overdoing supplements
Fiber supplements are convenient, but taking too much at once — especially without water — can worsen constipation, a common side effect of semaglutide.
Aim to get most of your fiber from food-based sources, and supplement with a small amount of supplemental fiber per day (such as 3–10 grams), unless directed otherwise by a provider.
Eating too much fiber when you have diarrhea
Fiber eases side effects like nausea and boosts feelings of fullness, making it easier to stick to your diet on semaglutide. But consuming too much of it when you have diarrhea (another common semaglutide side effect), or ramping up your fiber intake too quickly, can lead to more distress in the bathroom.
If you’re experiencing a lot of diarrhea on semaglutide, temporarily pull back on your fiber intake. Then gradually reintroduce more of it to your diet as your side effects subside.
Not drinking enough water
Fiber pulls water into your intestines, which can deplete your electrolyte levels if you’re not staying hydrated — especially on a medication like semaglutide that may reduce appetite and fluid intake.
Track your water intake throughout the day, especially in the early months when you’re dealing with side effects like nausea or constipation.
Sample Meal Plan (High-Fiber + Semaglutide-Friendly)
Want some fiber food inspiration? Here’s an example meal plan for someone on semaglutide aiming for fiber, fullness, and GI regularity.
Breakfast
- Oatmeal with ground flaxseed, chia seeds, and blueberries
- Green tea with lemon
- Optional: ginger chews to ease morning nausea
This fiber-rich breakfast sets you up for hours of fullness (based on my own personal experience) and tastes good, too.
Lunch
- Quinoa bowl with black beans, roasted sweet potatoes, kale, and avocado
- Water with lime
A hearty bowl filled with grains, veggies, and a healthy fat from avocado, this lunch is colorful and delicious.
Dinner
- Grilled salmon with a side of brown rice and sautéed spinach
- Baked apple slices with cinnamon for dessert
Lean proteins like fish are great for people on semaglutide, especially since fish is a good source of healthy unsaturated fat.
Snacks
- Apple with almond butter (pre-lunch)
- Air-popped popcorn (evening)
Hydrate throughout the day—aim for at least two liters (about 8.5 cups) of water total.
Bottom Line: Semaglutide and Fiber, Better Together
Semaglutide can be incredibly effective for weight loss. So can fiber. By improving gut health, controlling side effects, and working synergistically with your GLP-1, fiber can help you feel your best while shedding pounds.
Here’s what to remember:
- Add soluble fiber (like oats and psyllium) before meals to reduce appetite and support blood sugar.
- Use insoluble fiber (like brown rice and vegetables) to support regular bowel movements.
- Ramp up fiber slowly to avoid worsening diarrhea, gas, or bloating.
- Consider fiber supplements like psyllium husk or glucomannan if you have trouble getting enough fiber from your food.
- Hydrate often and frequently, getting at least 8 cups of water per day.
Talk to your healthcare provider or a registered dietitian to personalize your fiber plan on semaglutide.
Nutrition, fiber, and semaglutide each play an important role in your health, but the real results happen when they work together with the right support. At SkinnyRx, we offer compounded GLP-1 medications with clinical guidance. Take a short assessment to see if this approach could be right for you.


 Medically Reviewed
Medically Reviewed



