Key Takeaways
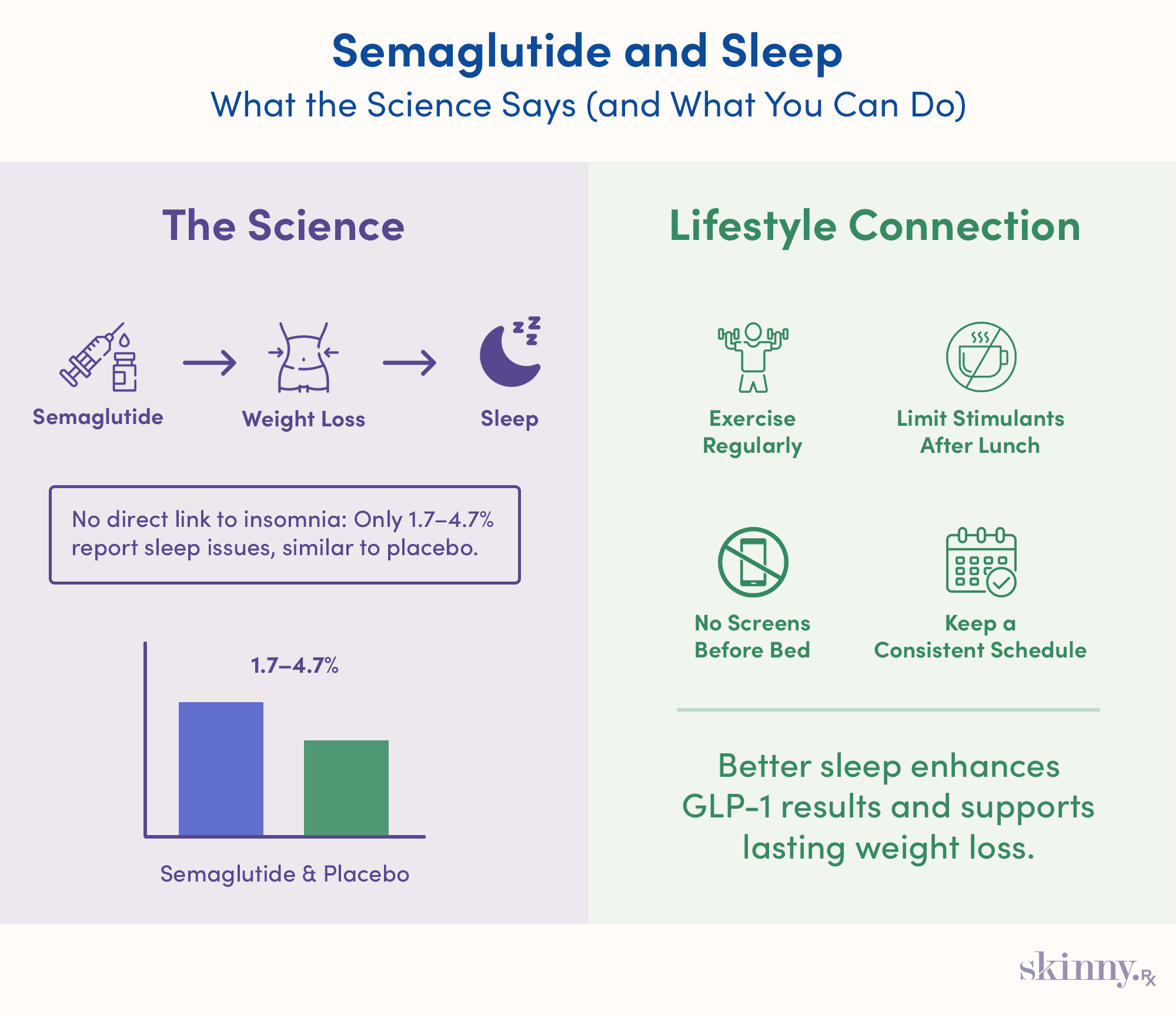
- Semaglutide is not directly linked to insomnia, and reported sleep issues occur at similar rates as placebo in clinical studies.
- Weight loss achieved through semaglutide can indirectly improve sleep quality and reduce the severity of sleep apnea.
- Poor sleep can hinder weight management efforts by affecting metabolism, appetite control, and energy balance.
- Lifestyle habits, such as regular exercise, avoiding caffeine late in the day, and limiting screen time, can significantly enhance sleep quality while taking semaglutide.
- Eating at least three hours before bedtime may help prevent reflux and improve sleep, as GLP-1 medications slow gastric emptying.
Here’s the deal: All medications have side effects. The severity of those side effects tend to correlate with the potency of the medicine itself, and semaglutide is a powerful tool for weight loss.
If you’re trying to change your health for the better, the last thing you need are restless nights. But when it comes to semaglutide and sleep, you can rest easy. According to a 2024 study covering thousands of subjects, semaglutide does not appear to be associated with an increased risk of adverse psychiatric conditions—insomnia included.
However, that’s not the whole story. Certain side effects of semaglutide can disrupt your sleep. Let’s walk through the details of sleeping on semaglutide and, more importantly, what to do if you’re taking the medication and struggling to get some shut-eye.
How Semaglutide Affects Sleep
Before we dive deeper, it’s important to contextualize the relationship between taking semaglutide and disordered sleep. While there isn’t a strong causal link between GLP-1 medications and sleep issues, some clinical data show that a small number of semaglutide users (1.7 to 4.7%) experience insomnia.
The same clinical review noted a similar prevalence of insomnia among those taking a placebo, which implies that the medicine itself does not directly cause or worsen chronic sleep issues.
The bigger question: can semaglutide actually help with sleep?
Semaglutide’s Positive Effects on Sleep
So, there isn’t much research indicating GLP-1 receptor agonists harm sleep habits on their own.
But there may be a positive correlation. A 2024 study in Japan of semaglutide users, measured over multiple years, concluded that “getting enough sleep may improve the weight loss effect of GLP-1 RAs in real-world settings.”
Moreover, with regard to improvements in sleep duration or quality for semaglutide users, it’s the outcome of the medicine itself—weight loss—that can really move the needle.
Semaglutide & Sleep Apnea
Semaglutide was originally developed to treat type 2 diabetes, a disease that commonly afflicts those suffering from obesity. Obese individuals are also at higher risk of developing sleep apnea, according to the Obesity Medicine Association.
Here’s where semaglutide shines: A 2025 meta-analysis (a bird’s eye examination of existing literature on a given topic) concluded GLP-1s could significantly reduce the prevalence of sleep apnea due to their research showing a threefold decrease in AHI, the medical metric used to measure how disruptive sleep apnea is on rest.
Other meta-analyses have made stronger claims. Also in 2025, Yang & colleagues alleged, “Patients with obesity and OSA may consider GLP-1 RA as a potential treatment option if the adverse effects are deemed tolerable.”

Expert-Guided, Sustainable Weight Loss
Discover how proven medications such as semaglutide or tirzepatide, combined with expert support, can help you reach lasting weight loss results.
Managing Sleep Issues on Semaglutide
Whether you’ve been diagnosed with sleep apnea or simply find yourself battling with bedtime on a nightly basis, you need practical solutions that may not involve taking more medication.
Neglecting your sleep hygiene—that is, habits and choices that influence the quality and consistency of your sleep—is essential, whether you’re taking semaglutide or not. Otherwise, you’re more likely to:
- Find it more difficult to maintain weight loss
- Have a weakened immune system
- Stray from a meal plan, or have a binge eating episode
It’s not hyperbolic to say that high-quality, regular sleep is a top priority for both weight loss and general health. Let’s run through some strategies that may help.
Lifestyle & Behavioral Strategies
When it comes to getting high-quality sleep, you may have to look beyond holistic solutions and consult with a medical professional, especially if you’re suffering from insomnia.
For improving mild sleep disruption, the beauty is in the basics: Buttoning up your holistic habits can improve the duration, consistency, and quality of your sleep. Here are some areas that need improvement.
Exercise Regularly
Sleep is restorative. It recovers losses suffered from both mental and physical stress. While we tend to experience plenty of mental load in our day-to-day lives, physical exertion isn’t as common.
Studies show frequent exercise has a positive effect on sleep habits. And it makes sense—a long day’s labor will have you out like a light once you hit the hay. If you don’t work with your hands or on your feet, dedicated bouts of low- to medium-intensity exercise should suffice.
Try two or three bouts of weekly strength training or moderate-intensity cardio like walking uphill, jogging, or circuit training. You should find that moving more both improves your daily energy and helps you fall asleep faster.
Limit Stimulants
A morning coffee is one thing, but an afternoon or evening cup might be doing your sleep serious harm. Here’s what most people don’t know—caffeine is famous for providing a quick jolt of alertness, but it continues to work in your system long after the jitters have subsided.
The data tell that caffeine can impede sleep up to 9 hours after ingestion, or as long as 13 hours if you consume a pre-workout supplement. A good rule of thumb here is to abstain from caffeine or stimulants after lunchtime.
No Screens in Bed
Screen usage has become so deeply embedded in our lifestyles that, in many cases, we hardly notice the disruptive effects that come with smartphones and other devices. Take their effects on sleep habits, for instance; a growing body of research is illustrating that keeping your smartphone out of the bedroom can assist with falling asleep.
Why? Due to such frequent usage, our brains rewire themselves to attend to the device, especially if it is within arm’s reach—making it all the more difficult to break away from the dopamine drip it provides.
More practically, studies show the artificial light emitted by smartphones and laptops suppresses your body’s production of melatonin, a hormone that eases you into the early stages of sleep.
Keep It Consistent
Consistency is key when it comes to managing your health, sleep included. And you shouldn’t let perfect be the enemy of good; regularity in your rest beats peaks and valleys every time.
Experts agree that sleeping and waking around the same time is essential for overall sleep hygiene and can help with your energy throughout the day. In a similar vein, you shouldn’t expect to “make up” for periods of missed sleep. Some data have shown that sleeping longer on certain days doesn’t counteract inconsistent or brief rest elsewhere in the week.
Regarding waking up, you might try what some doctors call the “two alarm system”—set one alarm 30 minutes before a second one. The first alarm should have a soft, melodic tone, meant to slowly pull you out of sleep. If necessary, the second alarm is there to ensure you get up.
Dietary Adjustments & Timing
You may also consider changing your dietary habits, especially if you’re a nocturnal eater. Some data suggest that eating 30-60 minutes before bedtime can negatively impact the ability to fall asleep, although this varies significantly from person to person.

For those having trouble sleeping while on a GLP-1 agonist, we will sometimes recommend our patients to stop eating anything, even 3 hours or more before bed. Because GLP-1 agonists can delay gastric emptying, some people need more time between eating before bed to sleep well, and this increased window without food can also help reduce nighttime reflux and heartburn symptoms, which are sometimes increased with GLP-1 use.
–
Dr. Daniel McGee, Board-certified Family Medicine Physician
If you tend to feel more relaxed with less food in your stomach, consider shifting your final meal of the day to take place at least three hours prior to your bedtime. Semaglutide delays gastric emptying even further, so it pays to give yourself extra leeway here.
Regarding what you eat, you should also be wary of large or carbohydrate-laden meals. Consuming simple carbs or sugars in bulk before bed can spike your blood sugar, making it difficult to relax enough to fall asleep, according to some research.
When To Talk To Your Doctor
If you’re on semaglutide and struggling to fall asleep, the medication is likely not to blame. Regardless, bouts of insomnia are unpleasant, stressful, and can seriously impede your weight loss efforts.
If you’ve been struggling to fall asleep for multiple weeks at a time, and at-home remedies aren’t doing the trick, consult with your healthcare provider.
At SkinnyRx, we offer doctor-guided access to compounded GLP-1 medications to help you reach your weight-loss goals safely and effectively. You can begin with a brief online assessment to determine if treatment is suitable for you.


 Medically Reviewed
Medically Reviewed